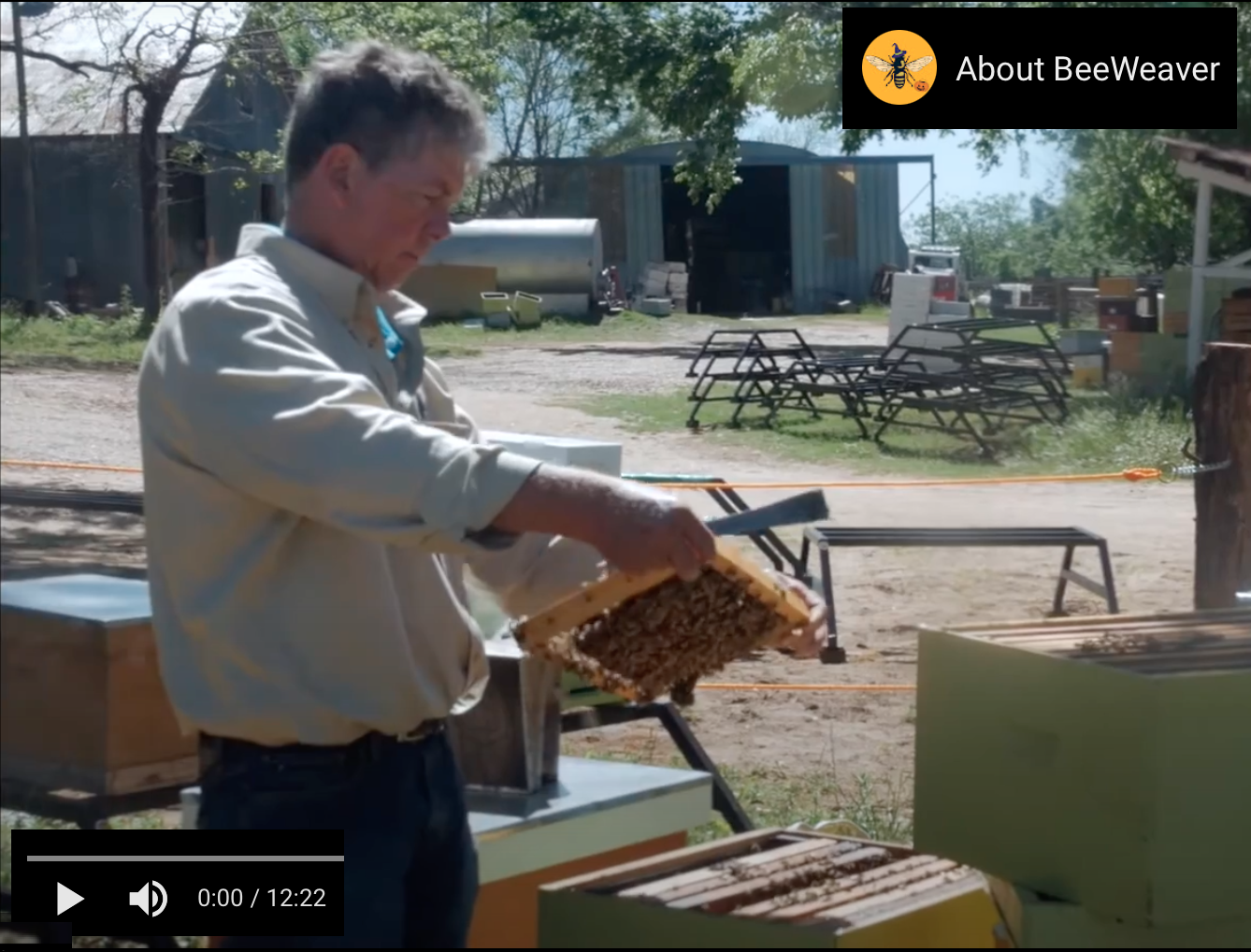
images : honeybee heart video
essay 1: *** Honeybee Heart ***
essay 2: *** Cardiology Origins ***
essay 3: *** History of Cardiology and Cardiovascular Surgery - Intersections in Alabama ***
Cardiology Origins - Past, Present, and Future of Cardiology and Cardiac Surgery ... *Intersections with UAB* - A Visual Tour - June 2018 presentation - PDF slideshow
external links:
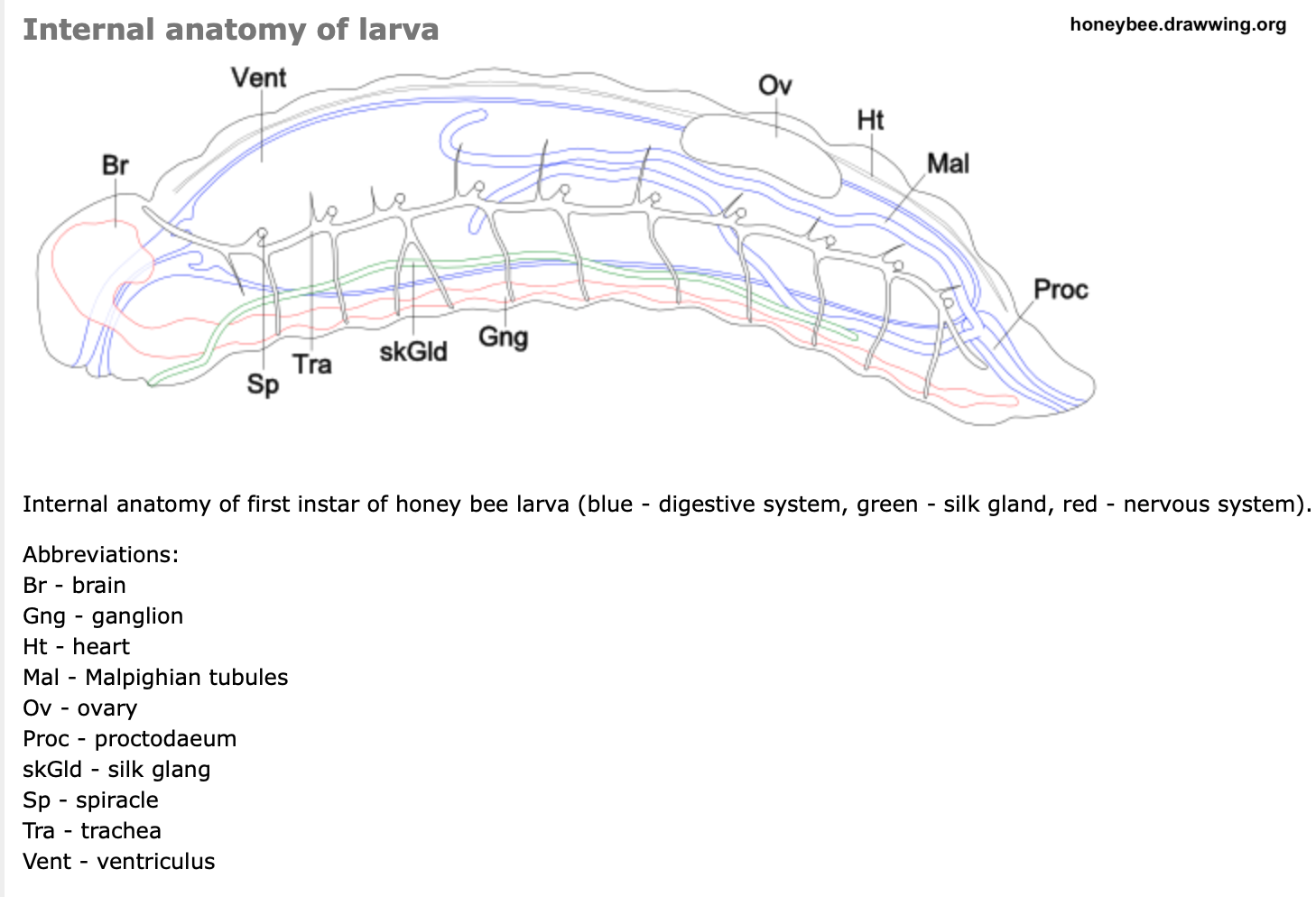
Dissection and Observation of Honey Bee Dorsal Vessel for Studies of Cardiac Function - Journal of Visualized Experiments - 2016
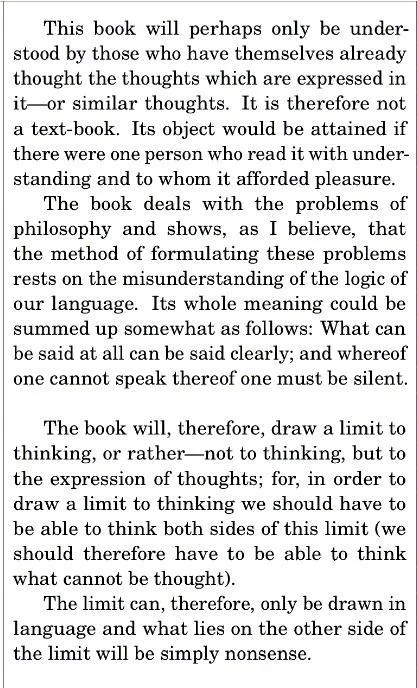
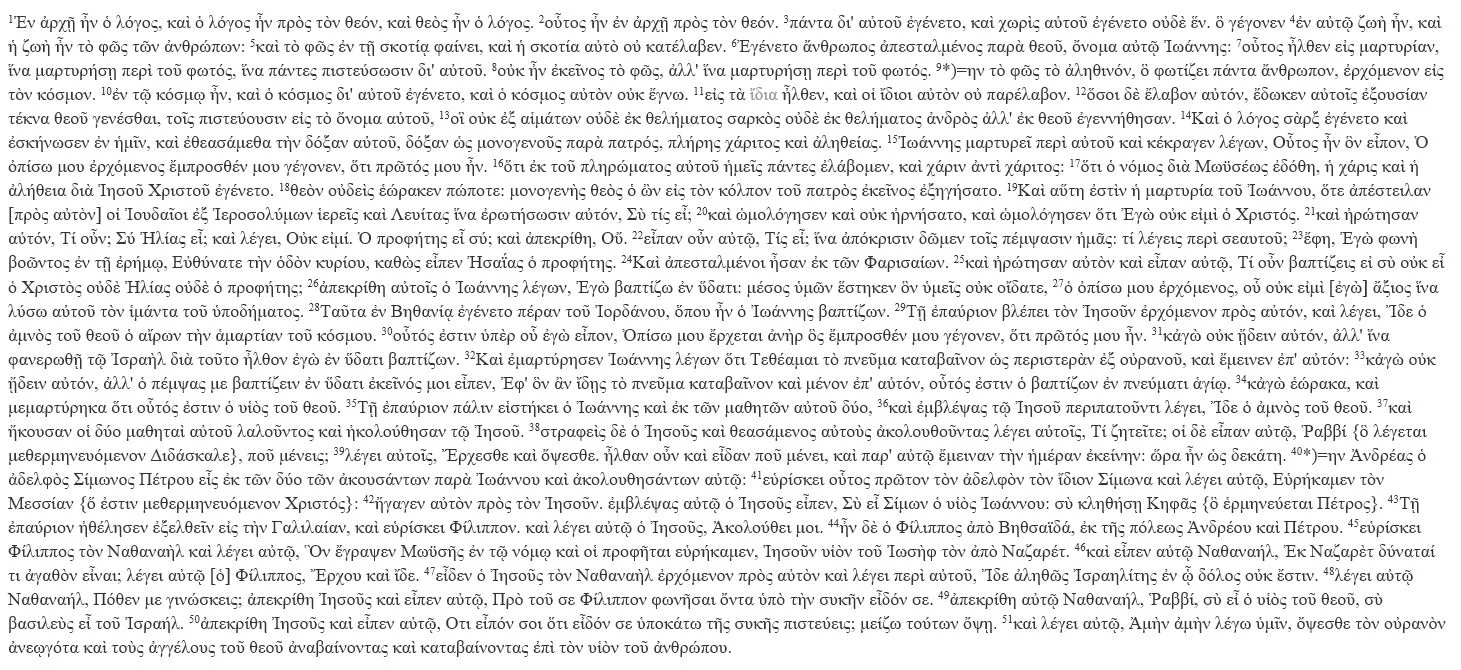
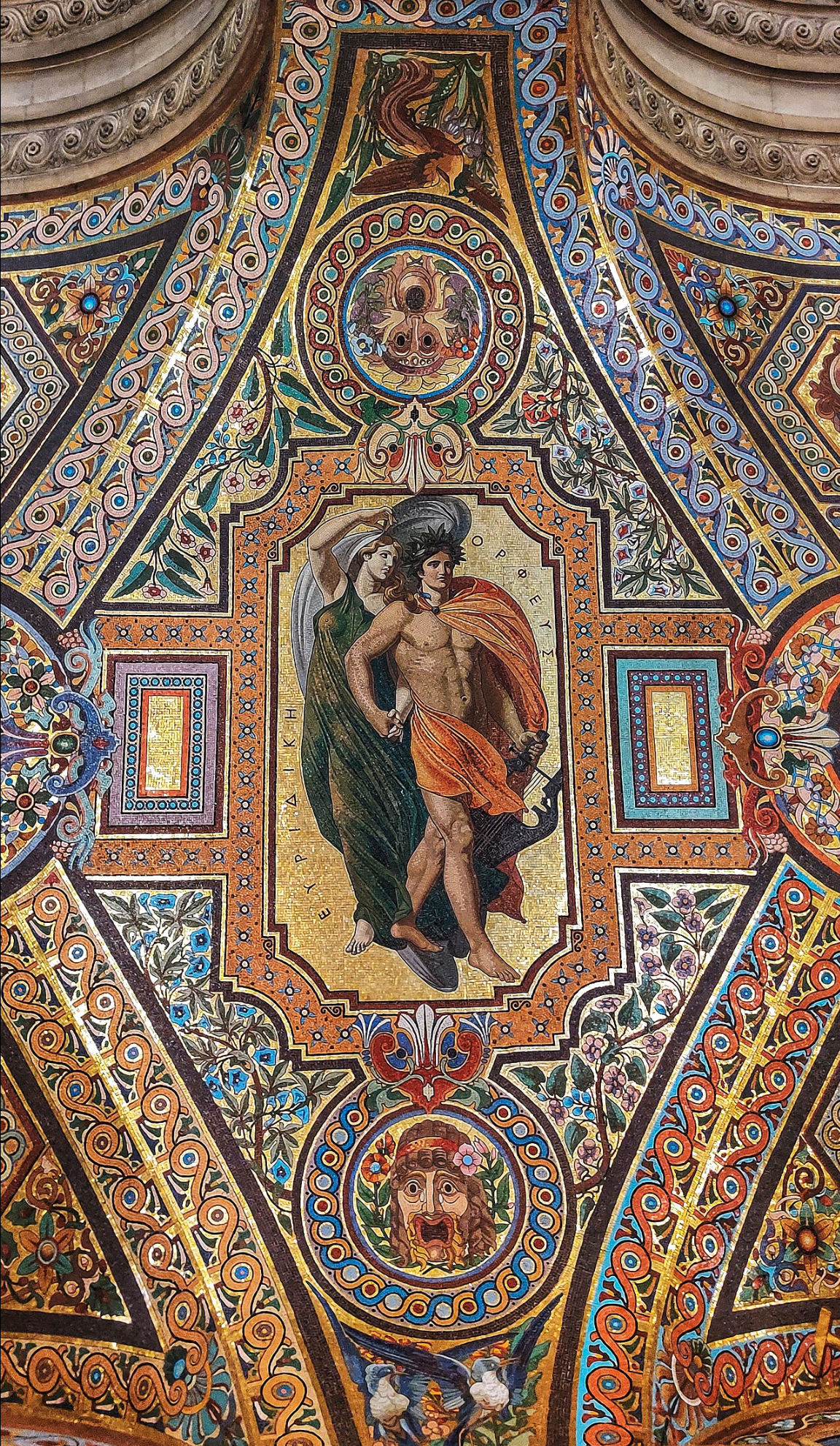
ΠΕΡΙ ΦΥΣΙΚΩΝ ΔΥΝΑΜΕΩΝ On the Natural Faculties - Galen - 150 AD [ complete text in Greek, with English translation ]
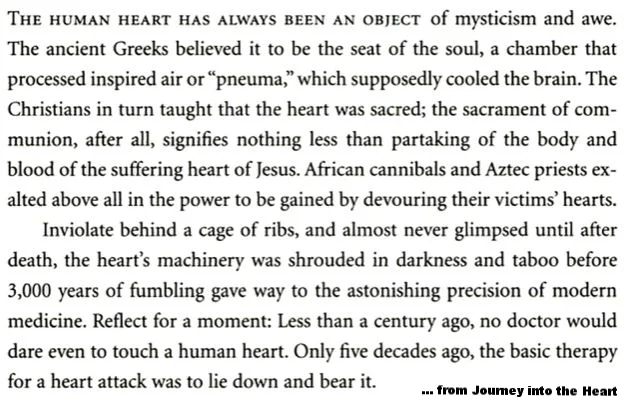
… from the Introduction:
“The ancient Greeks referred the origins of medicine to a god Asklepios, thereby testifying to their appreciation of the truly divine function of the healing art. The emblem of Aesculapius, familiar in medical symbolism at the present day, was a staff with a serpent coiled round it, the animal typifying wisdom in general, and more particularly the wisdom of the medicine-man, with his semi-miraculous powers over life and death.
“The temples of Aesculapius were scattered over the ancient Hellenic world. To them the sick and ailing resorted in crowds. The treatment, which was in the hands of an hereditary priesthood, combined the best of the methods carried on at our present-day health-resorts, our hydropathics, sanatoriums, and nursing-homes. Fresh air, water-cures, massage, gymnastics, psychotherapy, and natural methods in general were chiefly relied on.
“Hippocrates, the “Father of Medicine” (460 - 370 BC) was associated with the Asclepieum of Kos, an island off the south-west coast of Asia Minor, near Rhodes. He revitalized the work of the health-temples, which had before his time been showing a certain decline in vigour, coupled with a corresponding excessive tendency towards sophistry and priestcraft.
“Hippocrates first gave the physician an independent standing, separating him from the cosmological speculator. Hippocrates confined the medical man to medicine. He did with medical thought what Socrates did with thought in general—he “brought it down from heaven to earth.
‘Hippocrates set his face against any tendency to mystery-mongering, to exclusiveness. His concern was rather with the physician’s duties than his ‘rights.’
“At the dawn of recorded medical history Hippocrates stands for the fundamental and primary importance of *seeing clearly* — that is of clinical observation. And what he observed was that the human organism, when exposed to certain abnormal conditions — certain stresses — tends to behave in a certain way: that in other words, each “disease” tends to run a certain definite course. To him a disease was essentially a process, one and indivisible, and thus his practical problem was essentially one of prognosis — ‘What will be the natural course of this disease, if left to itself?’
“Vesalius (1514-64), known as the modern “Father of Anatomy,” for dissecting human bodies, was fiercely assailed by the hosts of orthodoxy. Vesalius proved that Galen had been wrong in saying that the interventricular septum of the heart was permeable.
“Michael Servetus (1509-53) suggested that the blood, in order to get from the right to the left side of the heart, might have to pass through the lungs. *For his heterodox opinions [regarding other matters] he was burned at the stake.
“William Harvey (1578-1657), who founded modern experimental physiology, was the first to establish not only the fact of the circulation but also the physical laws governing it, and is commonly reckoned the Father of Modern Medicine. He owed his interest in the movements of the blood to Fabricio, his tutor at Padua, who drew his attention to the valves in the veins, thus suggesting the idea of a *circular* as opposed to a to-and-fro motion. Harvey’s great generalisation, based upon a long series of experiments in vivo, gave the coup de grâce to Galenic physiology.
“*** Modern medicine, based upon a painstaking research into the details of physiological function, had begun. ***”
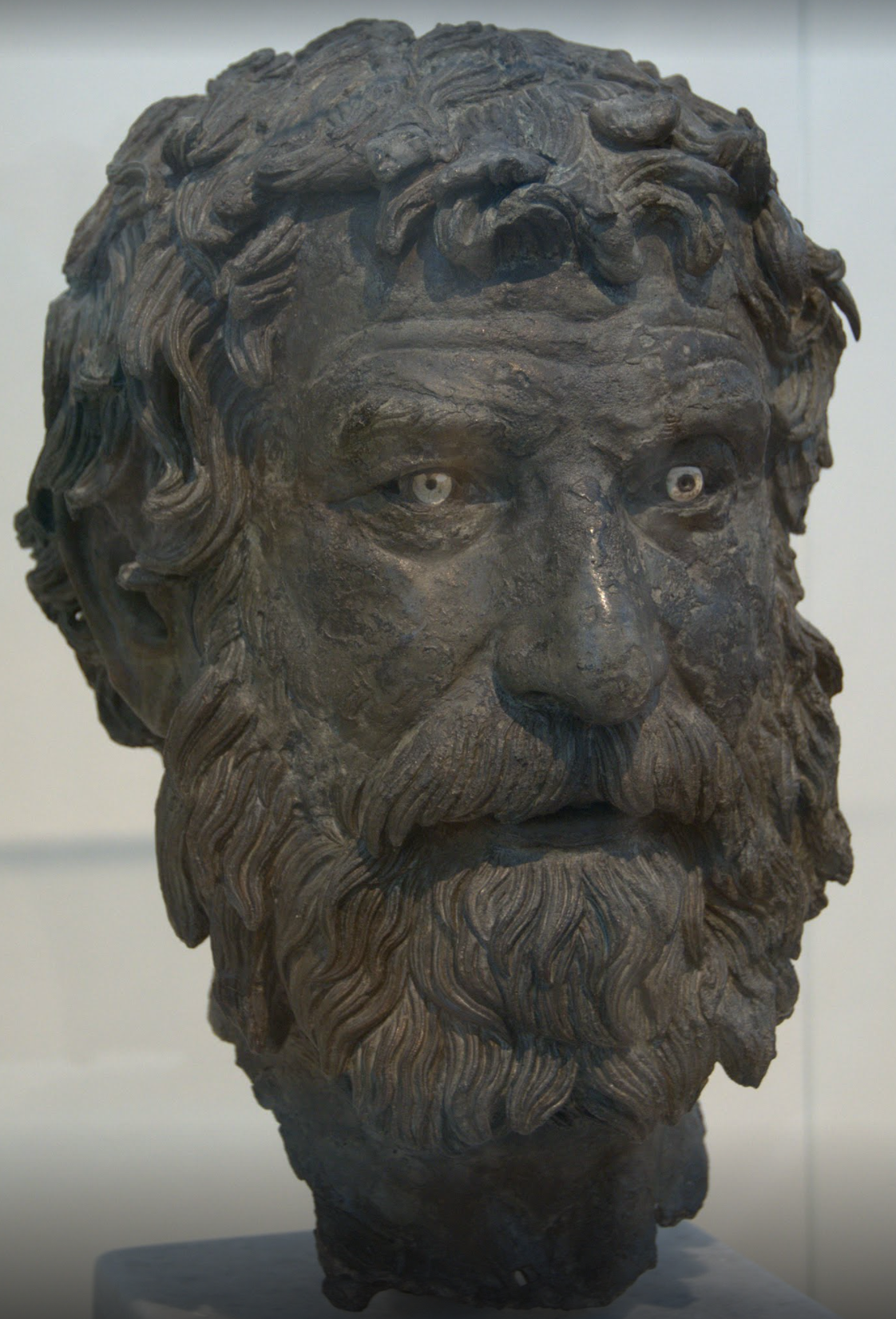
Re: Galen of Pergamon - 129-216 AD
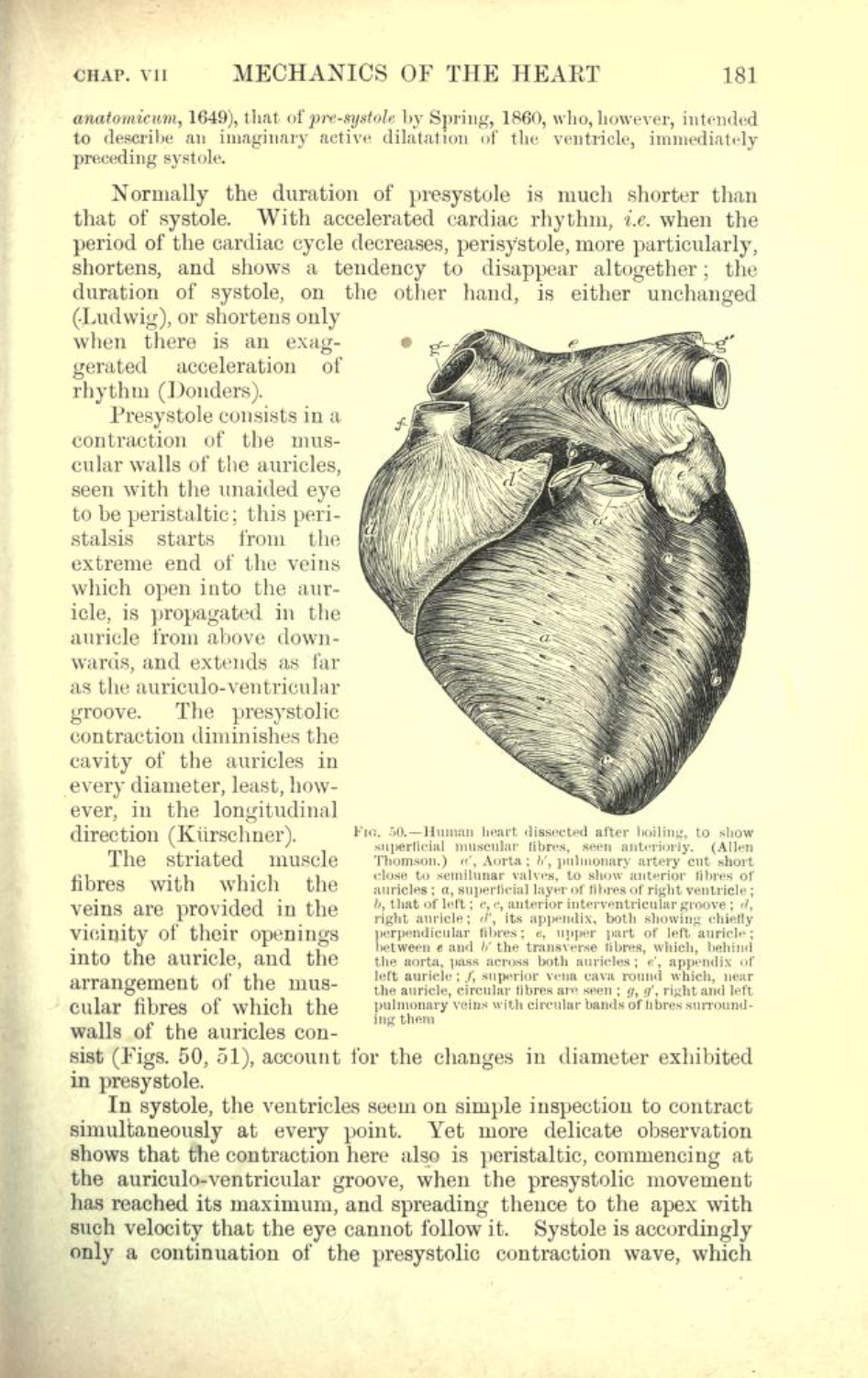
De Humani Corporis Fabrica - Cordis
De Humani Corporis Fabrica - Andreas Vesalius - 1543 - digital access to entire work
De Humani Corporis Fabrica : On the Fabric of the Human Body - 1543 - Andreas Vesalius - link to New Fabrica site
Re: Andreas Vesalius
Extensive sampling of pages from recently published New Fabrica
De Motu Cordis : Anatomical Studies on the Motion of the Heart and Blood - 1628 - William Harvey (complete text)
Re: William Harvey
In 1599, aged 21, he enrolled at the University of Padua in Italy, which was acclaimed for its medical and anatomy courses. (Interestingly, when Harvey arrived in Padua, Galileo Galilei had already been there for seven years, teaching mathematics, physics and astronomy.)
The greatest influence on Harvey at Padua University was his teacher, Hieronymus Fabricius, who was a skilled anatomist and surgeon. The two became friends and Harvey learned from Fabricius that dissection offered a route to better understanding of the human body.
Harvey made his discoveries because he ignored the conventional wisdom of medical text books, preferring to make his own observations and form his own conclusions when he dissected animals.
Remarkably, western medical beliefs and theories about blood and circulation had advanced little since Galen wrote his medical textbooks in Rome 1400 years earlier.
Lewis's Medical History of Alabama - Part One - The New Orleans Medical and Surgical Journal - May, 1847
Medical History of Alabama (continued) - The New Orleans Medical and Surgical Journal - July, 1847
New York Medical College - history - virtual timeline: 1849 - present
Arrowsmith - by Sinclair Lewis - 1925 - link to complete text
Our Medicine Men - by Paul de Kruif (microbiologist and scientific advisor to Sinclair Lewis) - 1922 - link to complete text
Microbe Hunters - by Paul de Kruif - 1926 - link to complete text
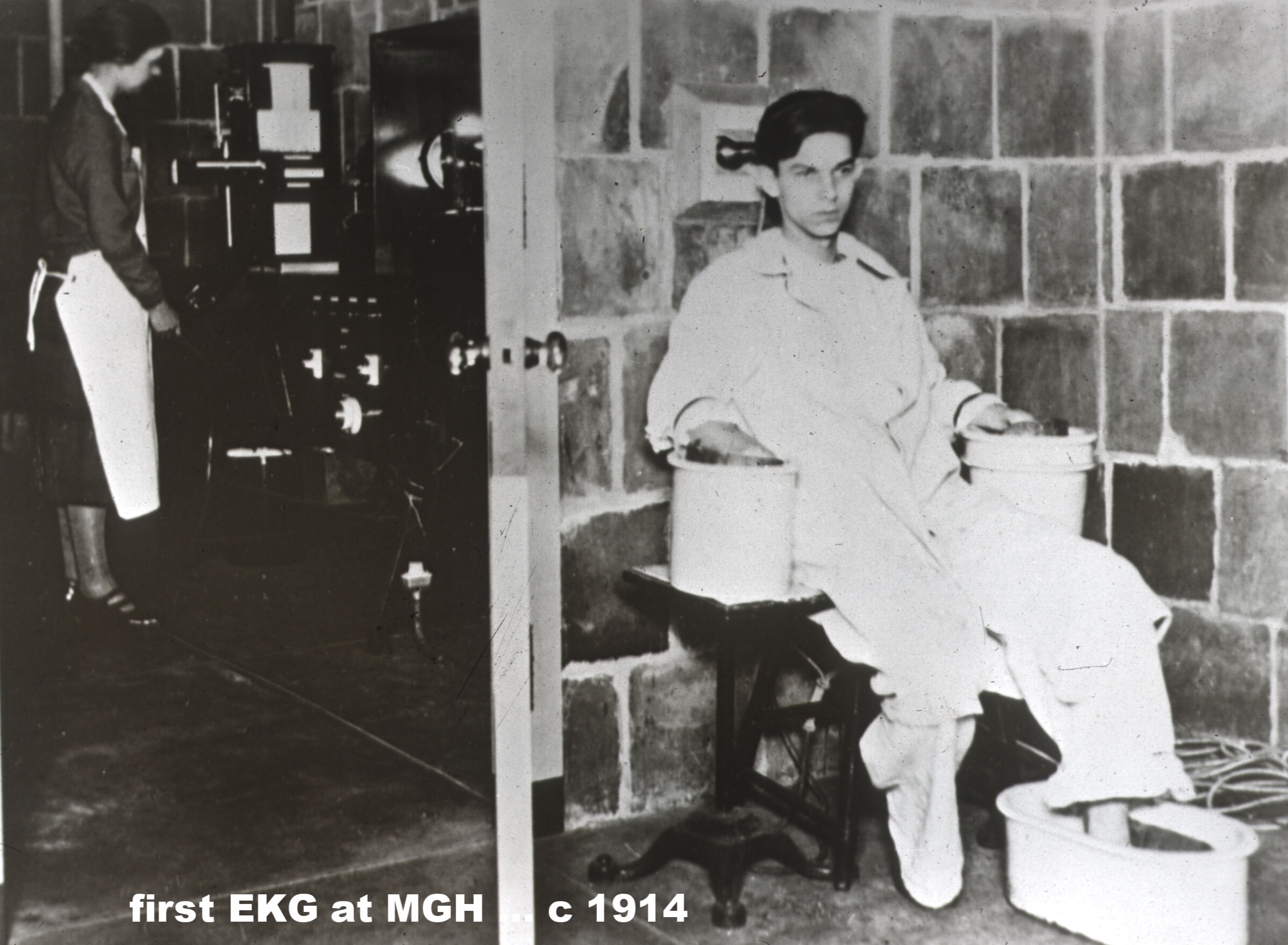
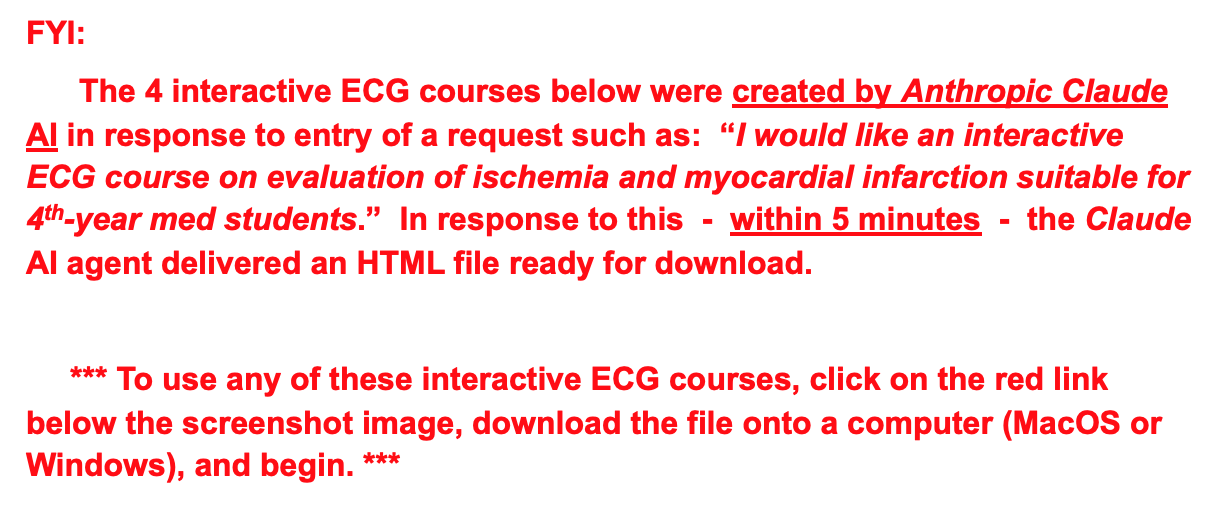
The Nobel Prize in Physiology or Medicine 1924 ... awarded to Willem Einthoven: In regard to Einthoven’s work, Professor J.E. Johansson, Chairman of the Nobel Committee for Physiology or Medicine of the Royal Caroline Institute, made the following statement:
“The Staff of Professors of the Royal Caroline Institute has on 23rd October, 1924, decided to confer this year’s Nobel Prize in Physiology or Medicine to the Professor of Physiology at the University of Leiden, Willem Einthoven, for his discovery of the mechanism of the electrocardiogram.
“Einthoven’s name is linked partly with the design of a physical instrument, the string galvanometer, partly with the so-called electrocardiogram, a record of the electrical potential fluctuations at the surface of the body, which accompany the heart beat. The heart beat, like the piston movement of a steam engine, is a cyclic process. Behind this process lies, in the first place, a similarly cyclic process in the heart muscle.
…
“The same mechanism governing the characteristics of the electrocardiogram, also governs the characteristics of the mechanical process during the heart beat. We should remember in this connection that the mechanical process not only consists of the succession of the stimulation of the separate parts of the heart compartments, but also of the cooperation of the individual parts of the heart wall which form the essential condition for the mechanical effect in the individual ventricle or in the individual auricle. A deficiency in this cooperation can, with regard to the mechanical effect, be as fatal as a valvular insufficiency. Today, the importance of the mechanism discovered by Einthoven can easily be realized.”
Paul Dudley White: The Father of American Cardiology*
History of Cardiology @ Massachusetts General Hospital
100 Years of Cardiology at MGH - AHA News article 12/6/16
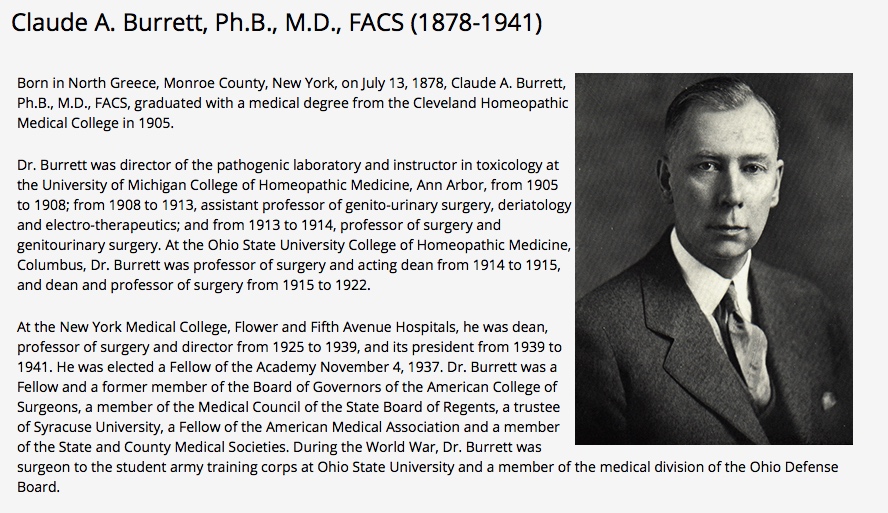
Claude A. Burrett - Dean / President, New York Medical College & Flower and Fifth Avenue Hospitals - 1939
Dr. Claude A. Burrett, NYT obit, March 5, 1941
John B. Burrett & Paul Dudley White - Am. Jour. Med. Sci. - March 1945
50 Years of Cardiology in Alabama - H. Duke Thomas - 1981
Foundations of Medicine and Surgery in Alabama and in Birmingham
- Kirby I Bland - Journal of the American College of Surgeons - April 2018
… from that article:
Fifteen miles to the northeast of Birmingham, the small city of Trussville, AL was the birthplace of brothers John Daniel Davis (b. 1859) and William Elias Davis (b. 1863). These brothers were the founders of the Alabama Surgical and Gynecological Association, which reorganized to become the Southern Surgical Association. The grandfather of the brothers was Dr. Daniel Elias Davis, who had moved from Abbeville, South Carolina to Tuscaloosa in 1848.
With recurring illness after high school graduation at age 16, John stayed home in Trussville and studied medicine in Birmingham with Dr M.H. Jordan. Soon after, an additional illness required his transition of study from Trussville to Montevallo and thereafter, Pleasant Hill, AL. John did not attend an undergraduate college. He entered medical school and graduated with a medical degree at age 20 from the Medical College of Georgia, in 1879.
After 2 years of local medical and surgical practice in Ferryville, AL, within contiguous St Clair County, John moved his home and practice, in 1881, to burgeoning Birmingham, providing opportunity for brother Elias to read medicine with him.
Young Elias was an exceptional and gifted student in all academic courses, so at age 19, he was prematurely admitted, in 1882, as a junior to the University of Alabama at Tuscaloosa. Like John, Elias did not obtain a college degree from the University for reasons of ill health and monetary deficits. Thereafter, Elias matriculated for the study of medicine at Vanderbilt University (1882), then the Kentucky School of Medicine (University of Louisville) (1883). Finally, Elias entered the Bellevue Hospital Medical College in New York City and graduated in the spring of 1884 with his medical degree, together with 149 classmates.
The synergy for the growth of medical practice and leadership in surgical sciences was evident when 21-year-old Elias joined brother John in the practice of surgery in downtown Birmingham after graduation.
The Davis brothers were strongly influenced by the clinical contributions of Ephraim McDowell (b. 1771), who was from Virginia and practiced in Kentucky. Additionally, the Alabama gynecologist, J. Marion Sims (b. 1813), born in South Carolina, practiced first at Mount Meigs, AL and afterward moved to Montgomery, where he practiced gynecology in the state from 1835 to 1853.
The Medical College of Alabama in Mobile, founded in 1859, was closed during the Civil War and did not reopen until 1868, when the Medical College faculty regained possession. Although post-Civil War lack of support of the infrastructure saw valuable laboratories and student education sites fall into dilapidation, and major organ specimens damaged or stolen, the greatest losses were among the ranks of the medical faculty killed and injured in the war. Others left impoverished Mobile for greater stipends in other cities and states.
At the recommendation of the Abraham Flexner report of 1910, the school moved to its new location at the University of Alabama in Tuscaloosa as a 2-year basic science school, with transfer of clinical students to out-of-state schools of medicine.
In 1945 the Medical College of Alabama moved to Birmingham and the newly constructed Jefferson Towers became the University Hospital for the University of Alabama in Birmingham (UAB) School of Medicine.
Werner Forssmann and Catheterization of the Heart, 1929 - Annals of Thoracic Surgery
Werner Forssmann, André Cournand, and Dickinson Richards - Nobel Prize for Medicine or Physiology - 1956
Werner Forssmann - Nobel Lecture - 12/11/56
… from his lecture:
“The ancient world and the Middle Ages had no idea of the existence of the circulation of the blood. It was not until the Late Renaissance that efforts were made to grasp this process anatomically and understand its function. Thus, Miguel Serveto searched in vain for a connection between the right heart and the left, and in so doing discovered the lesser circulation in 1553. In 1569, Caesalpinus traced the path of the large circulation. Jacobus Sylvius (1543), Canani (1564), and Fabricius of Aquapendente (1574) concurred in recognizing the centripetal movement of the venous bloodstream from the structure and arrangement of valves in the veins. Before their time it had been believed that blood flowed outwards to the periphery, even in the veins.
“William Harvey, one of the most gifted pupils of Fabricius (1578-1657), combined all these individual findings with the results of his own research to form the general picture of what we today call the circulation of the blood. But even he had no clear idea of the circulation in the region of the capillaries. This section was explained and described for the first time by Malpighi in 1661, after he had viewed a frog's lung under a microscope.
“In any event, it is the year 1628, in which Harvey published his classic work De motu cordis et sangunis, that we can call the birth-year of cardiology.”
An Investigator’s Journey in Cardiology - by Richard Bing - JAMA - 1992
Cardiac Cath Labs - Their Origin and Their Future - CHEST - 2018
Giants in Chest Medicine: Jim Dalen - CHEST - 2016 - video interview
A Chronological History of UAB Medicine
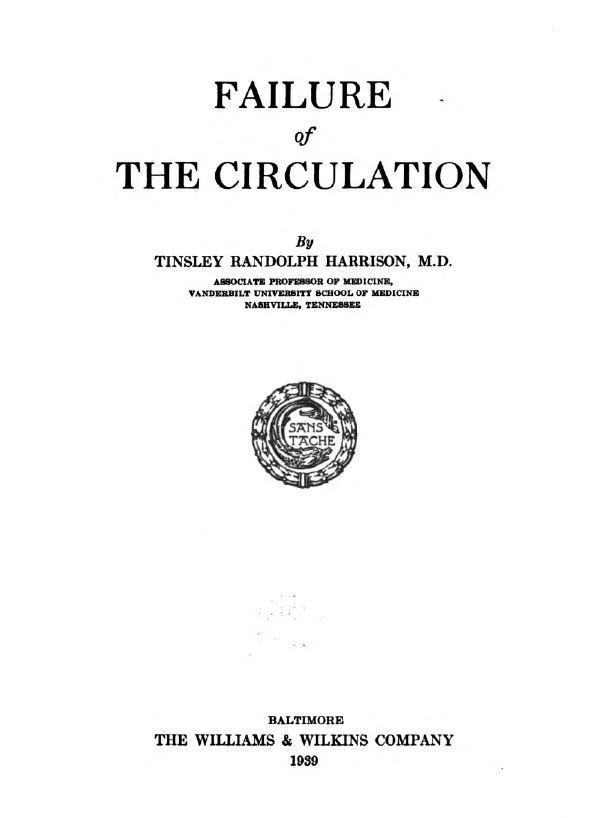
The Good Doctor: Tinsley R. Harrison - from MMI Archives
Tinsley R. Harrison | Encyclopedia of Alabama
Tinsley R. Harrison, M.D.: Teacher of Medicine - bio - by Jim Pittman - 2014
Tinsley Harrison, MD: Teacher of Medicine - notes, pics, timelines - PDF
The Principles of Therapy in Patients with Congestive Heart Failure - Tinsley R. Harrison, M.D. - NEJM - September 17, 1936
Vanderbilt Medicine - The Dynamic Duo - Al Blalock / Tinsley Harrison
Vivien Thomas audio interview (1967) - discussing work on HTN (in 1937-38): collaboration at Vanderbilt between Tinsley Harrison and Al Blalock
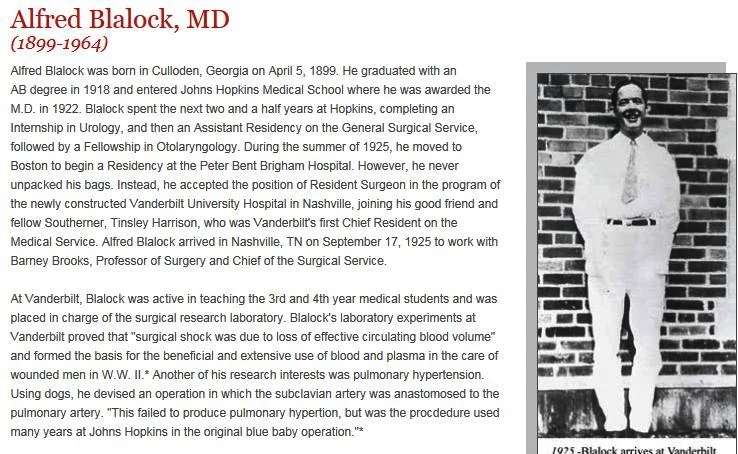
Alfred Blalock bio - J. Thoracic and Cardiovascular Surgery
Helen Taussig - bio
Johns Hopkins Medicine - history
First Operation - Taussig / Blalock / Thomas - Johns Hopkins archives
“By the third time the procedure was performed, the success of the operation had become dramatically apparent. Dr. Taussig described the third patient to receive the landmark operation "as an utterly miserable, small six-year old boy who was no longer able to walk." His skin was intensely blue, his lips deep purple. Just after the final stitches were tied and the clamps released, the anesthesiologist called out, "The boy's a lovely color now!" Dr. Taussig remembered the thrill of walking around to the head of the operating table to see those "lovely normal pink lips." She reported that after his recovery from the operation he was a happy, active child.
“In 1945, the first scientific paper describing the original three operations appeared in the Journal of the American Medical Association and had immediate worldwide impact.”
The Surgical Treatment of Malformations of the Heart - Blalock and Taussig - JAMA - May 19, 1945
Vivien Thomas helped develop the “blue baby” operation at Johns Hopkins - The Baltimore Sun - 2007
Vivien Thomas Pioneered Surgery That Saved Millions Of Lives- Investor's Business Daily - 2016
Like Something the Lord Made:
“Internal healing of the incision was without flaw. The sutures could not be seen from within, and on gross examination the edges of the defect were smooth and covered with endocardium. Dr. Blalock finally broke the silence by asking, 'Vivien, are you sure you did this?’ I answered in the affirmative, and then after a pause he said, `Well, this looks like something the Lord made.’” - re Vivien Thomas ... National Magazine Award-winning 1989 article from Washingtonian
”Say his name, and the busiest heart surgeons in the world will stop and talk for an hour. Of course they have time, they say, these men who count time in seconds, who race against the clock. This is about Vivien Thomas. For Vivien they’ll make time.
Dr. Denton Cooley has just come out of surgery, and he has 47 minutes between operations. “No, you don’t need an appointment,” his secretary is saying. “Dr. Cooley’s right here. He wants to talk to you now.”
Cooley suddenly is on the line from his Texas Heart Institute in Houston. In a slow Texas drawl he says he just loves being bothered about Vivien. And then, in 47 minutes—just about the time it takes him to do a triple bypass—he tells you about the man who taught him that kind of speed.
No, Vivien Thomas wasn’t a doctor, says Cooley. He wasn’t even a college graduate. He was just so smart, and so skilled, and so much his own man, that it didn’t matter.
And could he operate. Even if you’d never seen surgery before, Cooley says, you could do it because Vivien made it look so simple.
Vivien Thomas and Denton Cooley both arrived at Baltimore’s Johns Hopkins Hospital in 1941— Cooley to begin work on his medical degree, Thomas to run the hospital’s surgical lab under Dr. Alfred Blalock. In 1941 the only other black employees at the Johns Hopkins Hospital were janitors. People stopped and stared at Thomas, flying down corridors in his white lab coat. Visitors’ eyes widened at the sight of a black man running the lab. But ultimately the fact that Thomas was black didn’t matter, either. What mattered was that Alfred Blalock and Vivien Thomas could do historic things together that neither could do alone.
Together they devised an operation to save “Blue Babies”—infants born with a heart defect that sends blood past their lungs—and Cooley was there, as an intern, for the first one. He remembers the tension in the operating room that November morning in 1944 as Dr. Blalock rebuilt a little girl’s tiny, twisted heart.”
Denton Cooley writes (see linked article):
‘‘Al, Eileen’s lips are a glorious pink color!’’ said Helen Taussig, MD, pediatrician at Johns Hopkins noted for congenital cardiac anomalies, excitedly. Were these words comparable to those of astronaut Neil Armstrong, ‘‘one giant leap for mankind’’ in introducing an era in human courage and exploration? As a participant in the surgical event at Johns Hopkins Hospital on November 29, 1944, and at the invitation of Lawrence Cohn, Editor of this Journal, I will relate some recollections of the historic first ‘‘blue baby’’ correction, which many consider the dawn of cardiac surgery.
By an unusual stroke of my personal luck, Dr. Alfred Blalock had witnessed a tennis game in the courtyard at Hopkins’ Hospital between me and a fellow third-year student, Lester Persky. To my surprise, he then invited me to join him and his family for a weekend at Gibson Island so that he could have an opponent for ping pong. That may have helped me as an aspiring surgeon. I served externships in surgery during my senior year to fill vacancies, as many of the house staff volunteered for military service during World War II.
After graduation from Hopkins School of Medicine, I received a personal invitation to join the surgical house staff as an intern.Having graduated on August 18, 1944, I joined the staff immediately for a straight surgical internship. My first rotation then was to provide fluid, blood, and plasma to support procedures in the operating rooms. That included responsibility for the blood bank and crossmatching of blood. I worked with one technician who enjoyed permanent employment. On the date of November 29, I arrived in scrub suit at 6:00 AM in the operating room for the scheduled procedure. Vivien Thomas, who was Dr Blalock’s trusted technician from the Hunterian Laboratory (the dog lab), was there already. An air of tension was felt by all.
The patient, Eileen Saxon, a 2-year-old intensely cyanotic and frail child, was chosen as the first patient for trial of a new and untested treatment for a congenital anomaly called tetralogy of Fallot. Most members of the medical and surgical staff questioned the plan to operate on this pathetic child.
Dr. Blalock took his position on the left side of the table, with Bill Longmire on the opposite side. Vivien stood behind Dr Blalock. Dr Taussig stood behind Harmel but was unable to witness the dissection. The incision was an anterolateral incision in the third interspace, and the second and third costal cartilages were divided. Exposure was limited by the incision, and I was unable to observe much. Because the aortic arch was on the left side, the subclavian artery was almost too short to pass over the arch into the left subclavian artery. Instruments were crude by today’s standards and consisted of several bulldog clamps, which were encircled with silk threads to permit traction. Some of these techniques had been developed by Vivien in the dog lab. Dissection in the highly vascular mediastinum to isolate the left pulmonary artery was skillfully done by Dr Blalock with instruments and his left index finger. When the final preparation for the anastomosis was made, the end of the shortened subclavian artery was connected with fine black silk sutures to the side of the pulmonary artery. Dr Blalock several times asked Vivien for advice on suturing.
Vivien T. Thomas : an oral history [sound recording] / interviewed by Peter D. Olch, Apr. 20, 1967 - NIH / US National Library of Medicine - mp3 audio file and transcript
The Blalock-Taussig-Thomas Collaboration - JAMA - 7/16/08
* Something the Lord Made - Alfred Blalock / Vivien Thomas * ... movie trailer … link to movie on HBOmax
A Change of Heart: Vivien Thomas and the Blue Baby - excellent 10 -min. video documentary told by a patient.
Something the Lord Made - Alfred Blalock / Vivien Thomas... movie review
Vivien Thomas - New Iberia, Louisiana-> Nashville -> Vanderbilt/Blalock -> Johns Hopkins/Blalock
Re: Vivien Thomas - bio
Partners of the Heart: Impact Proposal
Partners of the Heart- movie trailer
Saving our Doomed "Blue" Babies - The American Weekly, Feb., 1946
To Touch the Heart: Touch, Spiritual Anatomy, and Image Theory in Michelangelo's Noli Me Tangere
Noli Me Tangere (Michelangelo) - image
The first Blalock-Taussig shunt - by Dr. Denton Cooley, surgical intern in Hopkins O.R. on Nov. 29, 1944 - from Journal of Thoracic and Cardiovascular Surgery, Oct. 2010
From Johns Hopkins archives:
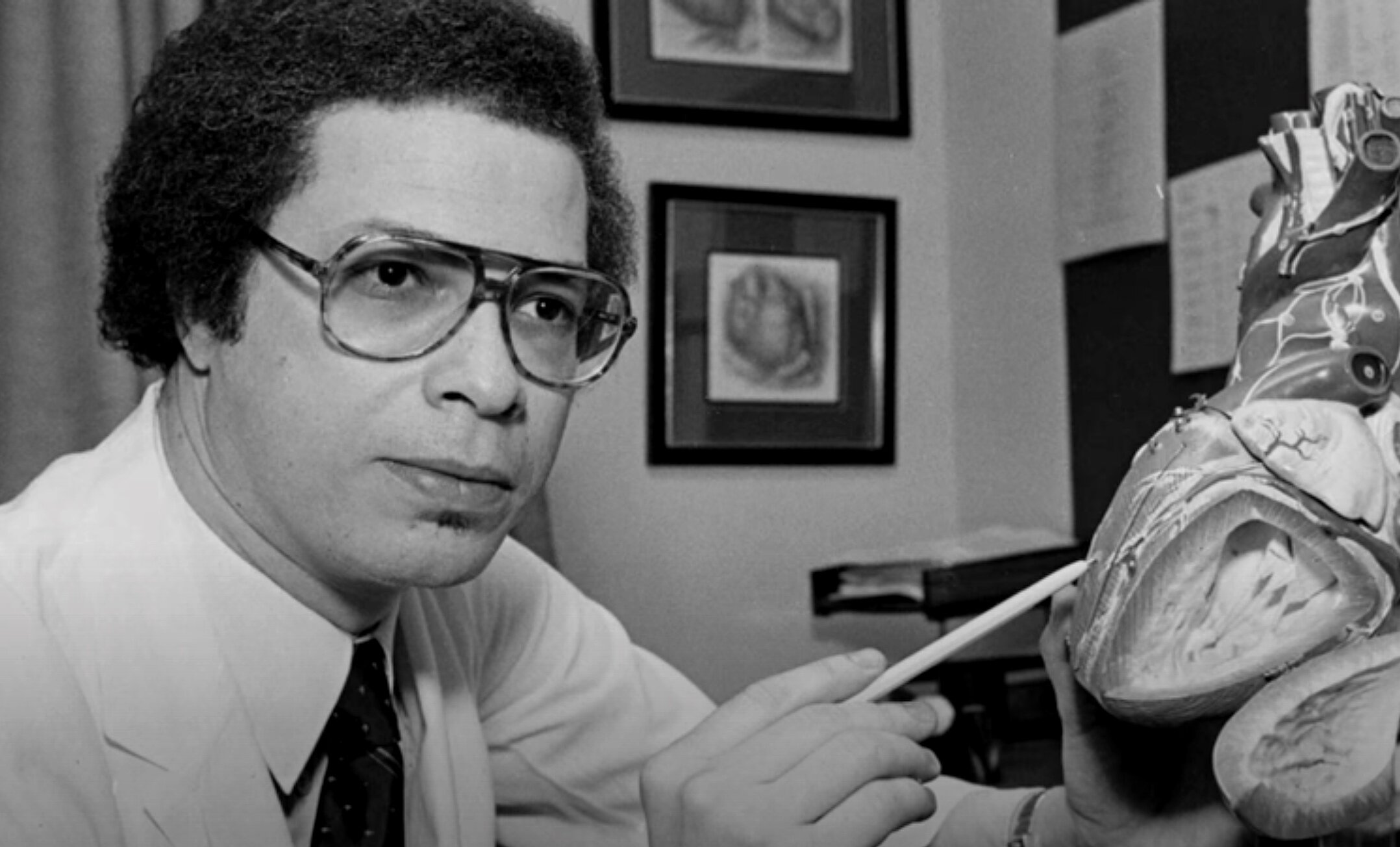
At Johns Hopkins, Vivien Thomas collaborated with Alfred Blalock and Helen Taussig to devise the operative technique to correct a congenital heart defect, Tetralogy of Fallot, or “Blue Baby Syndrome” that robs the blood of oxygen. First performed in 1944, the anastomosis operation named the Blalock-Taussig Shunt, brought fame to Blalock and Taussig. Vivien Thomas had worked out the surgical technique in the dog lab, using a clamp of his own design, and coached Blalock in the operating room through the first human operation.
As supervisor of the surgical laboratories for over 35 years, Thomas went on to train a generation of surgeons at Johns Hopkins in the delicate techniques necessary for heart and lung operations. Notable among them was Hopkins’ first black cardiac resident Levi Watkins, Jr, who was a pioneer in the use of the automatic implantable defibrillator, performing the first human operation in 1980, after having first tested the device on dogs with Thomas in his lab.
.
Champ Lyons - Brief life of an innovative surgeon: 1907-1965 - Harvard Magazine - 2016
Champ Lyons, Holt McDowell, and the Evolution of Vascular Surgery at the University of Alabama at Birmingham: A Personal Perspective - The American Surgeon - 2010
Champ Lyons, MD - The Ochsner Years: 1945 - 1950 - The Ochsner Journal - 2009
Evolution of Cardiopulmonary Bypass - Circulation
Blalock -> Kirklin in the development of open heart surgery
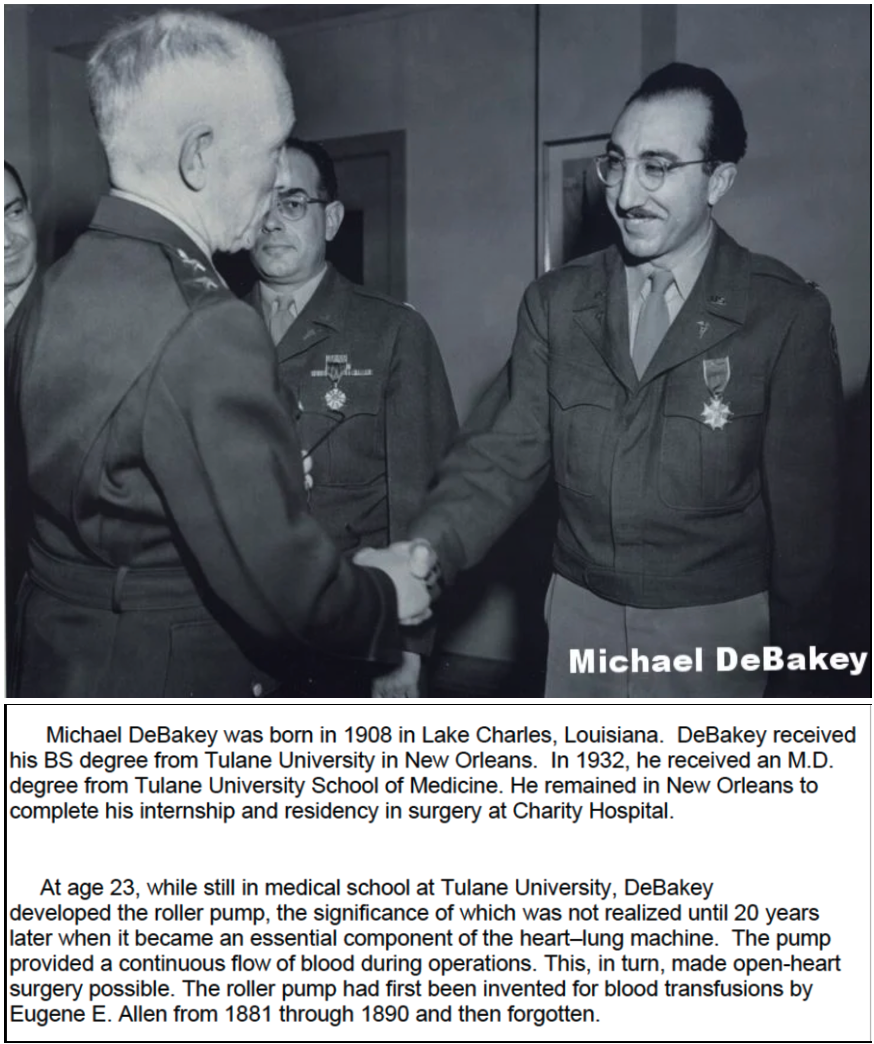
The Michael E. DeBakey Papers: from Tulane School of Medicine to the U.S. Army, 1928-1946
“In medical school, DeBakey worked for a professor who was researching arterial pulse waves. Asked to find or devise a pump that could modify such waves, DeBakey immersed himself in the engineering literature. He found several designs for roller pumps, which could propel fluid through rubber tubing held in a circular frame by pressing the tube with rollers, and soon built a small, hand-cranked version of his own. This worked well for his professor, but DeBakey realized that his roller pump would also be ideal for doing blood transfusions. At the time, transfusions were often done by collecting blood from the donor in a glass container, then quickly administering it to the patient, before it could clot. (Sodium citrate had been used as an anticoagulant for transfused blood since World War I, but it sometimes had severe side effects and many physicians preferred not to use it.) DeBakey's simple device made it possible to gently pump blood directly from donor to recipient, leaving less time for the blood to clot. And, having no valves, the roller pump did only minimal damage to the blood cells. DeBakey did thousands of transfusions for the New Orleans medical community using the pump.
“At a medical meeting a few years later, DeBakey met John Gibbon, who was developing the first heart-lung bypass machine. One of Gibbon's chief problems was the pump he used, which tended to destroy blood cells. DeBakey suggested his roller pump, and Gibbon incorporated a motorized version of it into his second prototype in the late 1930s. Modified versions of the DeBakey pump are still used in modern heart-lung machines.
“The Tulane mentors who had the greatest influence on DeBakey were Rudolph Matas (1860-1957) and Alton Ochsner (1896-1981). Matas, who retired as Chair of the Department of Surgery in 1927, was one of the outstanding surgeons of his time. William Osler called him "the father of vascular surgery" for his early work on peripheral aneurysm repair. Alton Ochsner succeeded Matas as head of the Department of Surgery, and quickly developed one of the best surgical teaching programs in America. Because Tulane didn't have its own hospital, the program was run from the New Orleans Charity Hospital. Ochsner was a pioneer in the surgical treatment of lung cancer and was one of the first to link lung and esophageal cancers to cigarette smoking.
“DeBakey met Ochsner during his third year of medical school, and in his fourth year began working in Ochsner's surgical laboratory, investigating peptic ulcer. He was soon in charge of the lab, sometimes doing eight to ten dog surgeries each day. He loved the research and technical aspects of operating, and was easily persuaded to continue in surgery as Ochsner's intern and then resident. After receiving his MD in 1932, DeBakey did his surgical residency at Charity Hospital, gradually becoming Ochsner's collaborator.
“When the United States entered World War II, DeBakey, like most young men, wanted to enter military service. Ochsner wanted to keep him at Tulane and initially declared him as "essential personnel," but then relented. DeBakey was immediately recruited to Surgical Consultants Division of the Army Surgeon General's office by his colleague Fred Rankin, who was then the Chief Consultant. Together with B. Noland Carter, DeBakey and Rankin were responsible for providing the Surgeon General with recommendations concerning all aspects of optimal care for the surgical needs of army personnel.”
Michael DeBakey - Leading Medicine - Methodist Hospital - 2003
HISTORICAL DEVELOPMENT OF CARDIOPULMONARY BYPASS
On May 6, 1953, the first successful truly open-heart operation was performed with the use of the heart-lung machine. On that spring day in Philadelphia, John Heysham Gibbon of the Jefferson University Medical Center, using total cardiopulmonary bypass for 26 minutes, closed a large secundum atrial septal defect (ASD) in an 18-year-old woman. Beginning with this case, generations of cardiac surgeons have been able to operate on millions of human hearts.
John W. Kirklin, M.D. - brief bio - Circulation 2004
John W. Kirklin and colleagues at the Mayo Clinic launched their open heart program on March 5, 1955. They used a heart-lung machine based on the Gibbon-IBM machine, but with their own modifications.
Dr. Kirklin wrote: " In the winter of 1954 and 1955 we had 9 surviving dogs out of 10 cardiopulmonary bypass runs. With my wonderful colleague and pediatric cardiologist, Jim DuShane, we had earlier selected 8 patients for intracardiac repair. Two had to be put off because two babies with very serious congenital heart disease came along and we decided to fit them into the schedule. We had determined to do all 8 patients even if the first 7 died. All of this was planned with the knowledge and approval of the governance of the Mayo Clinic. Our plan was then to return to the laboratory and spend the next 6 to 12 months solving the problems that had arisen in the first planned clinical trial of a pump oxygenator ... We did our first open heart operation on a Tuesday in March 1955."
Studies in Extracorporeal Circulation. I. Applicability of Gibbon-Type Pump-Oxygenator to Human Intracardiac Surgery: 40 Cases - John Kirklin et al. - Annals of Surgery - 1956
John Kirklin became Chairman of the Department of Surgery at the Mayo Clinic in 1960 and became Chairman of Surgery at the University of Alabama Birmingham in 1966. He served as Editor for The Journal of Thoracic and Cardiovascular Surgery, authored more than 500 scientific articles, and coauthored (with Sir Brian Barrett-Boyes) the definitive text Cardiac Surgery.
John W. Kirklin - bio - Profiles in Cardiology
Denton Cooley - Texas Heart pioneer - excellent 5 min. video
The Past 50 Years of Cardiovascular Surgery - Denton Cooley - Circulation - 2000
Fifty Years of Open Heart Surgery at the Mayo Clinic - Mayo Clinic Proceedings - 2005
Jimmy Kimmel’s Emotional Monologue: His New Son’s Heart Condition - NYT - May 1, 2017 ... infant son born in Apri with tetralogy of Fallot - video segment from Late Night
Tetralogy of Fallot explained: brief video
Moss & Adams' Heart Disease in Infants, Children, and Adolescents
Levi Watkins - bio from PBS documentary - Alabama -> Tennessee ... Vanderbilt -> Johns Hopkins
Termination of Malignant Ventricular Arrhythmias with an Implanted Automatic Defibrillator in Human Beings - 1980 - NEJM
Re: Levi Watkins - Baltimore Sun - April 2015
Levi Watkins bio and videos - Johns Hopkins site
All Heart - article reviewing tenure of Dr. Levi Watkins at Johns Hopkins School of Medicine
Lillian Watkins, 96: Wife of legendary Alabama State University president Levi Watkins, matriarch of accomplished Watkins family
“Her son, Dr. Levi Watkins, Jr., was the first African-American to graduate from Vanderbilt University and, in 1980, the first cardiac surgeon in the nation to perform a human implantation of the automatic implantable defibrillator.”
All Heart - 2013 article - brief bio of Dr. Levi Watkins, Jr.
Levi Watkins, 70, Dies - NYT obit - 4/16/15
Remembering Levi Watkins, Jr. - Vanderbilt U. article - 2015
Dr. Selwyn Vickers - Dean, UAB School of Medicine - honors Dr. Levi Watkins - Johns Hopkins Medicine - 2 min. video [re: Selwyn Vickers]
Profile: Selwyn Vickers, M.D., FACS
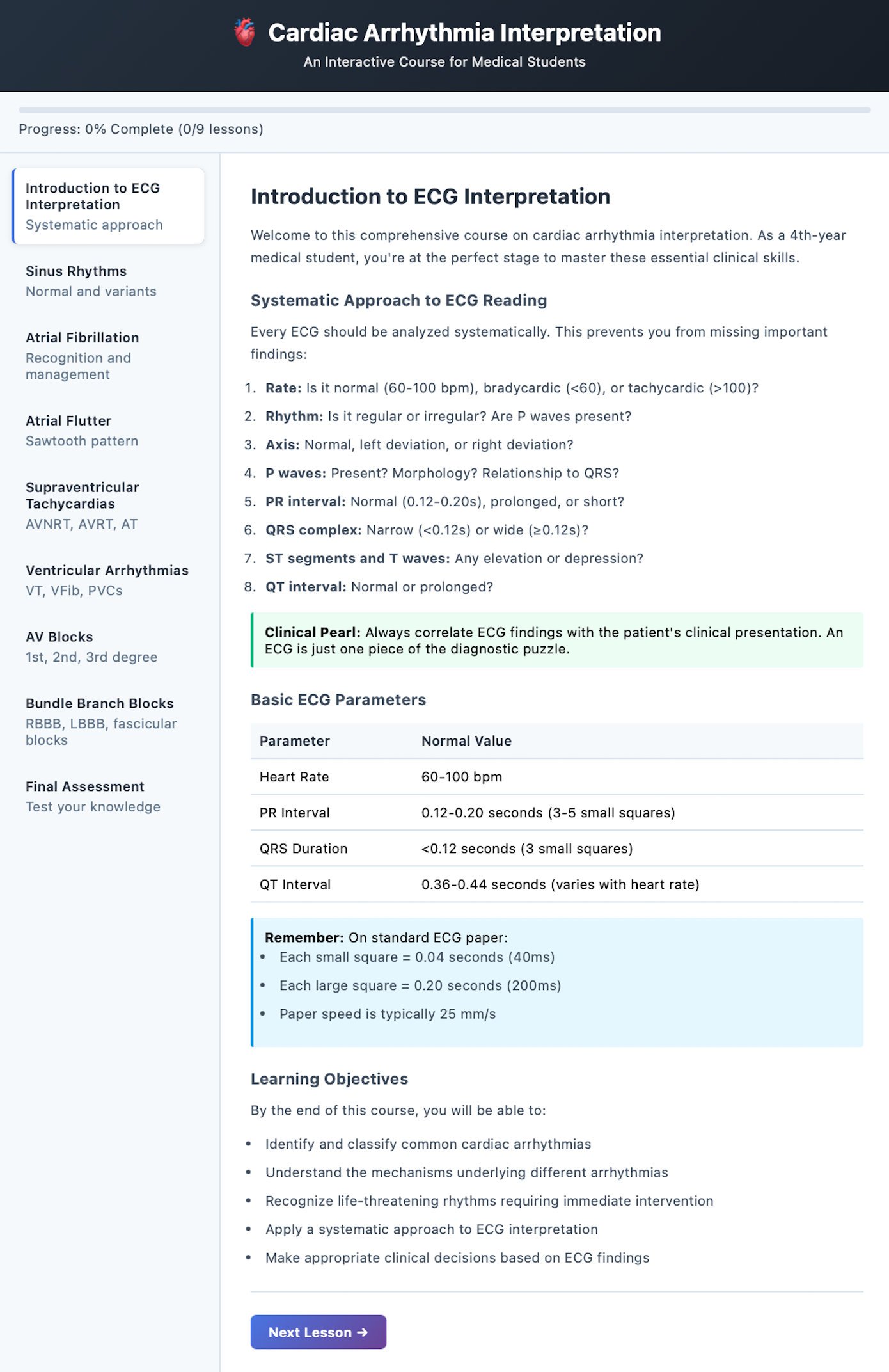
Cardiology: The Past, the Present, and the Future - 2003 Simon Dack Lecture - E. Braunwald
An Interview with Dr. Eugene Braunwald - Clinical Chemistry - 2012
Leaders in Cardiovascular Medicine - Eugene Braunwald: an interview - European Heart Journal - 2015
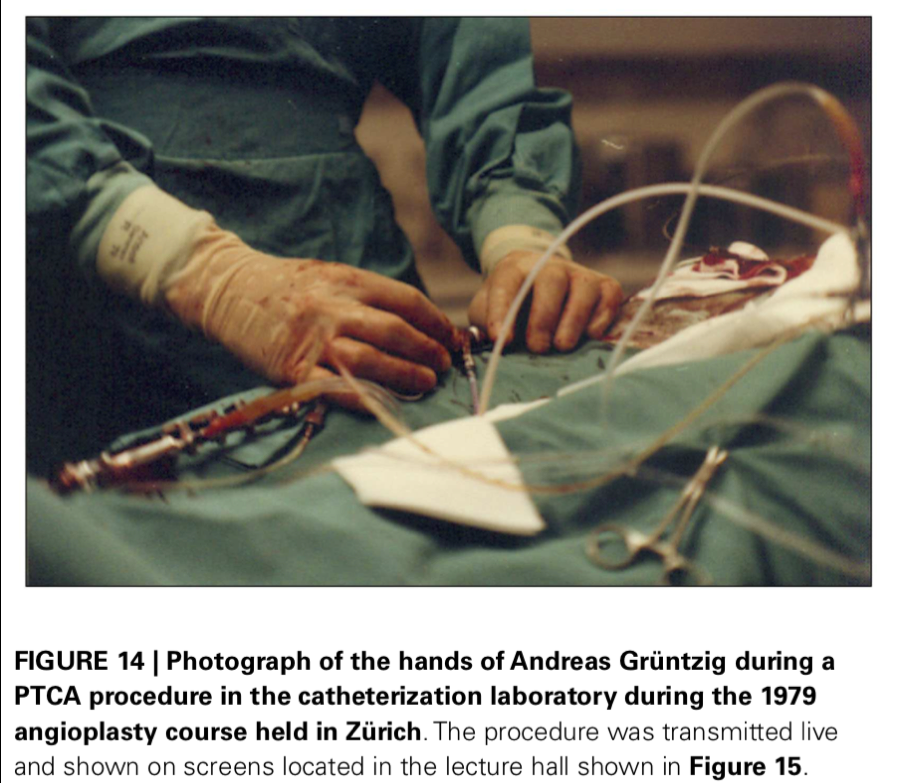
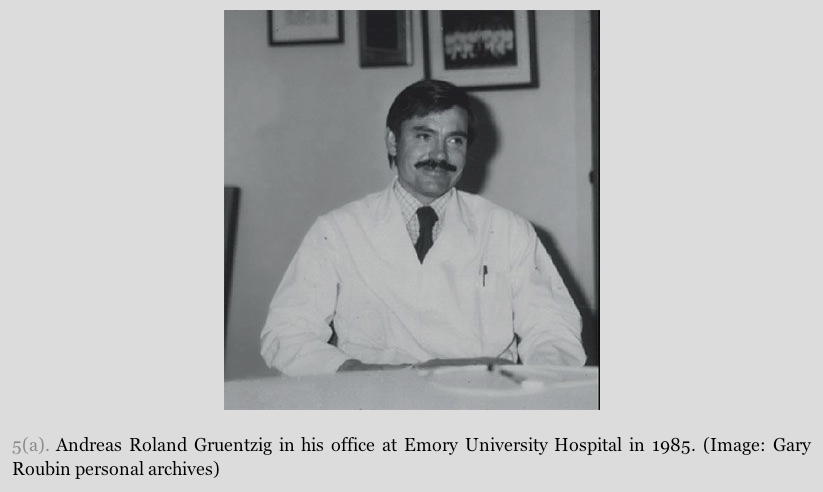
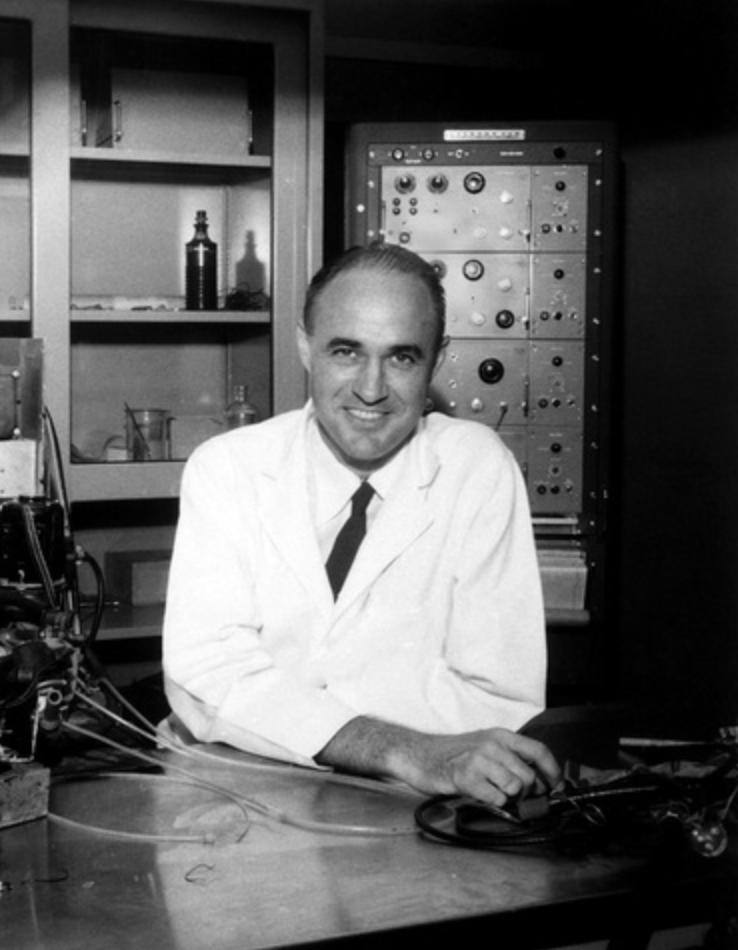
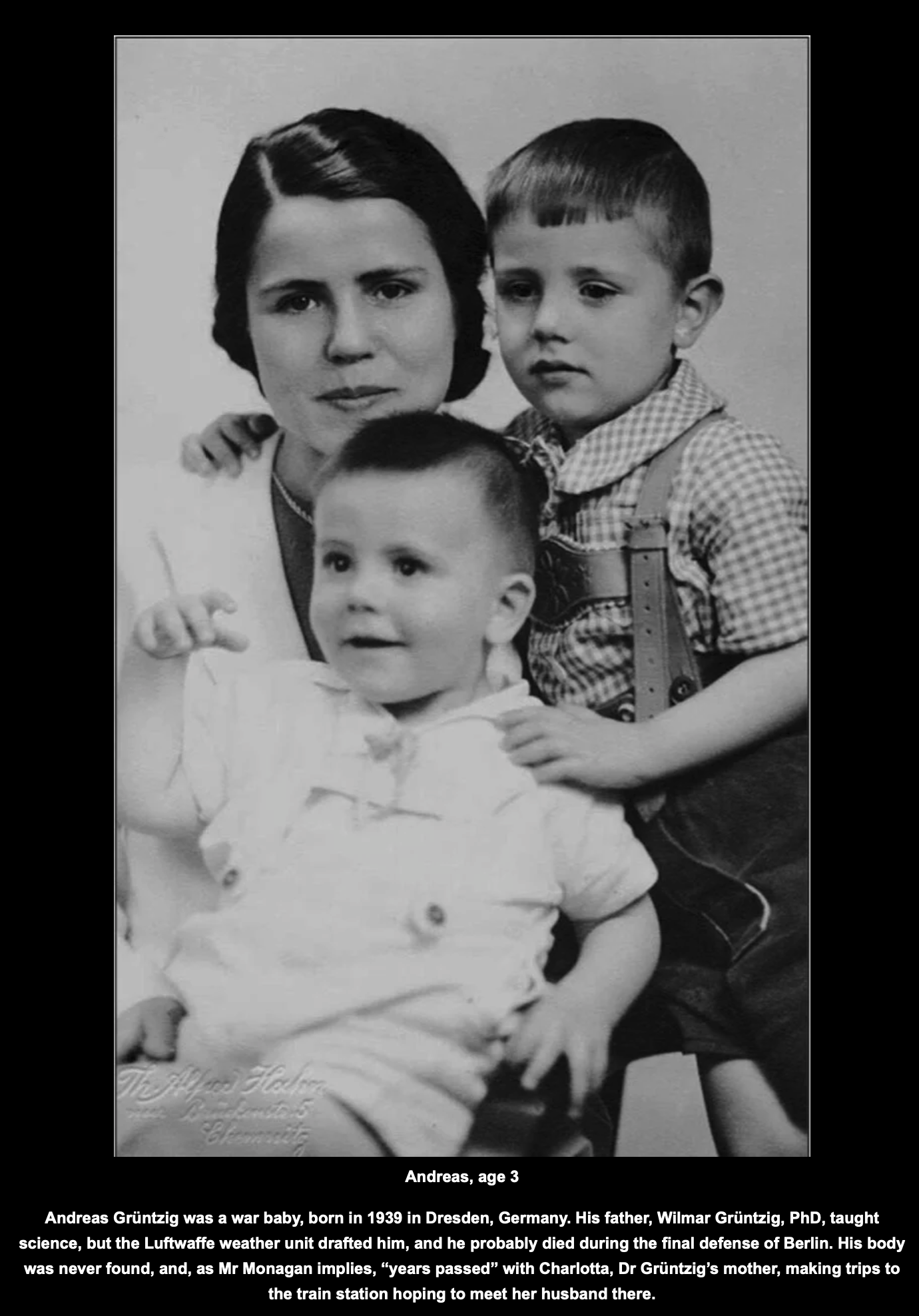
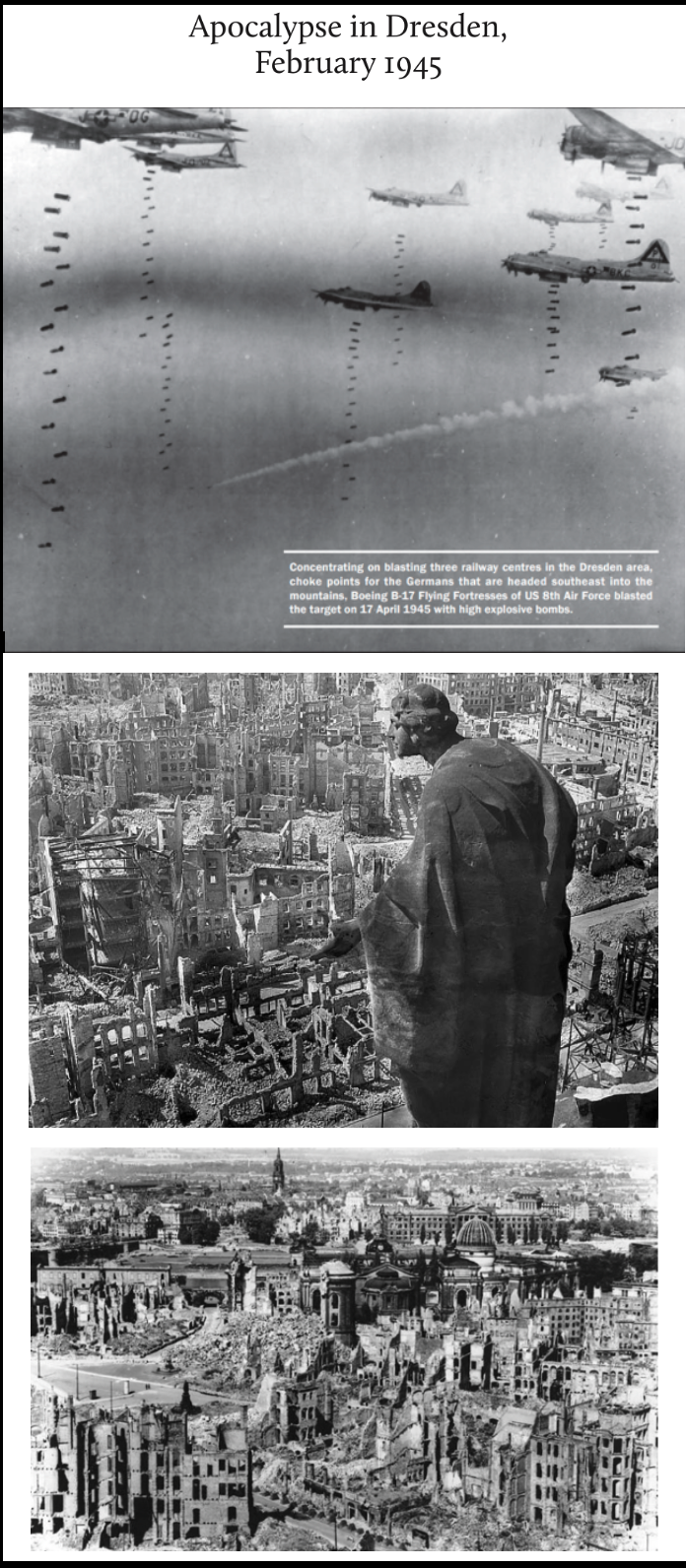
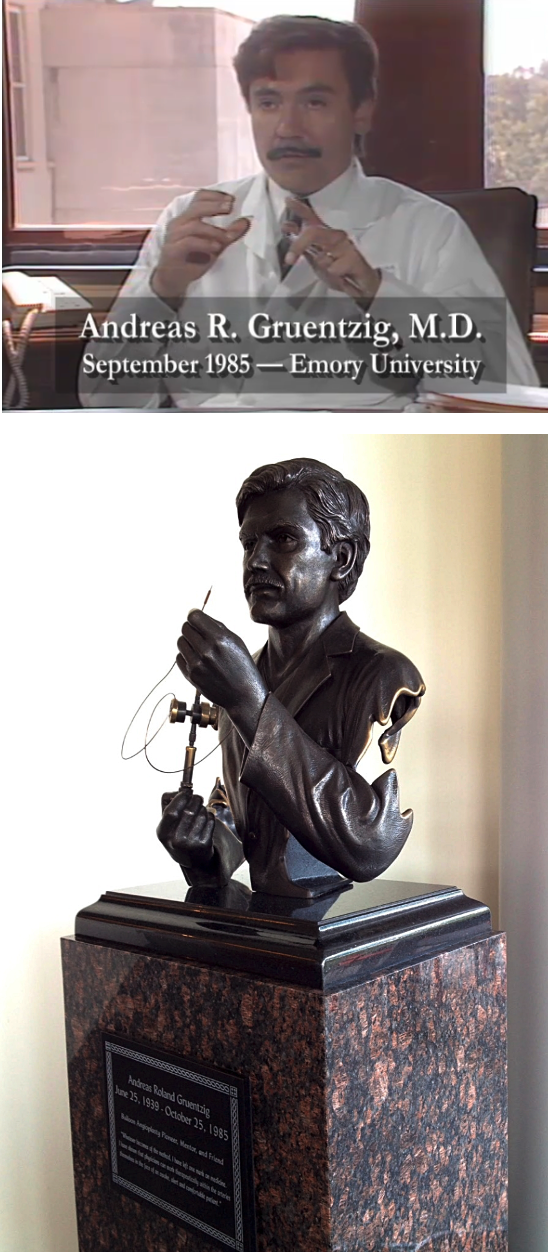
Andreas Grüntzig - 1977: First Coronary Angioplasty- bio - AHA Circulation - 2007
Andreas Gruentzig: The Teaching Genius - article by J. Willis Hurst
The First Balloon-Expandable Coronary Stent - An Expedition That Changed Cardiovascular Medicine - A Memoir - by Gary Roubin - 2015
The Beat Goes On: 50 Years of Heart Health (beginnings of modern CABG at the Cleveland Clinic) - NYT post
Texas Heart Institute: *Ray C. Fish Award for Scientific Achievement* - recipients from 1972 to present
My Life After a Heart Attack at 38 - NYT Opinion - 2019
“About half of people who die of a heart attack do so in the first hour. If not properly treated within that “golden hour,” heart muscle begins to die. Within six hours, if the heart attack hasn’t yet been fatal, victims face the possibility of irreversible damage. I didn’t get to the hospital until more than six hours after I felt the most acute pain. Despite my obvious signs of distress, I hesitated to go for help because it seemed inconvenient: My wife was scheduled to go on a work trip that morning, and my daughter had summer camp. It hadn’t fully clicked that what I was experiencing was an actual heart attack.
“In an instant I joined the group of about 805,000 Americans who suffer a heart attack each year (one every 40 seconds), including 605,000 who are struck for the first time. Heart disease is the No. 1 killer in America, responsible for one in four deaths.”
Centre of Excellence: Division of Cardiology, Leuven, Belgium - Circulation - 2008
A Brief History of Cardiac Pacing - 2006 - Images in Pediatric Cardiology
Extracorporeal Circulatory Support in the UAB Cath Lab: The TandemHeart Percutaneous Ventricular Assist Device - Cath Lab Digest - 2007
UAB Insight - on Heart and Vascular Disease - vol. 1, no. 1 2009
Cardiothoracic Surgery at UAB - 2010 video
UAB Hybrid O.R. - TAVR Procedure #500 - at UAB - 2016 video
Risk factor analysis from more than 6,000 mechanical circulatory support patients - James K. Kirklin et al. - Journal of Heart and Lung Transplantation - 2013
Frontier research: tissue engineering to repair damaged myocardium - brief animation video demonstrating concept
Patching the Heart - Cardiac Repair From Within and Outside - 2013 review article - Circulation - Zhang et al
Engineering Tissue for Cardiac Repair - Zhang - UAB
Cardiac Repair of Myocardial Infarction Using Human Stem Cells - Cell Stem Cell - 2014
A Large Scale Investigation of Hypoxia-Preconditioned Allogeneic Mesenchymal Stem Cells for Myocardial Repair in Nonhuman Primates - Circulation Research - 2016
Heme oxygenase-1 regulates mitochondrial quality control in the heart - JCI Insight - 2016
UAB Researchers Take on 5 Key Areas of Cardiovascular Disease - Medscape - 2016
Cardiac Tissue Chips (CTCs) for Modelling Cardiovascular Disease - Transactions on Biomedical Engineering - 2019
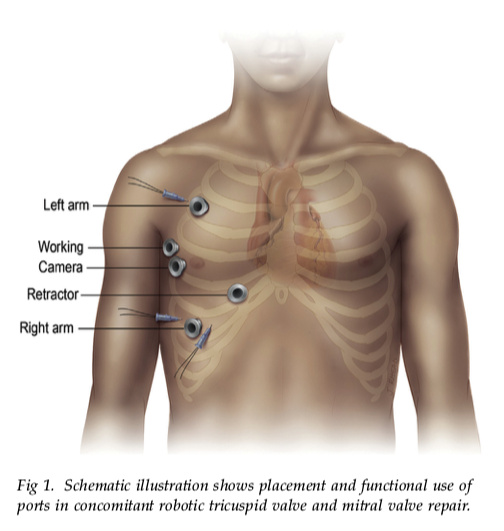
Robotic Cardiac Surgery: State of the Art in 2014 - part I - video
Robotic Cardiac Surgery: State of the Art in 2014 - part II - video
500th Robotic Cardiac Surgery at U. Chicago - video - 2017
Robot-assisted aortic valve surgery: State of the art and challenges for the future - International Journal of Medical Robotics - review - 2018
TAVR: Transcather Aortic Valve Replacement - UAB info and videos
MitraClip: Transcatheter Repair of Mitral Regurgitation - video
Anatomy of the pig heart: comparisons with normal human cardiac structure - Journal of Anatomy - 1998
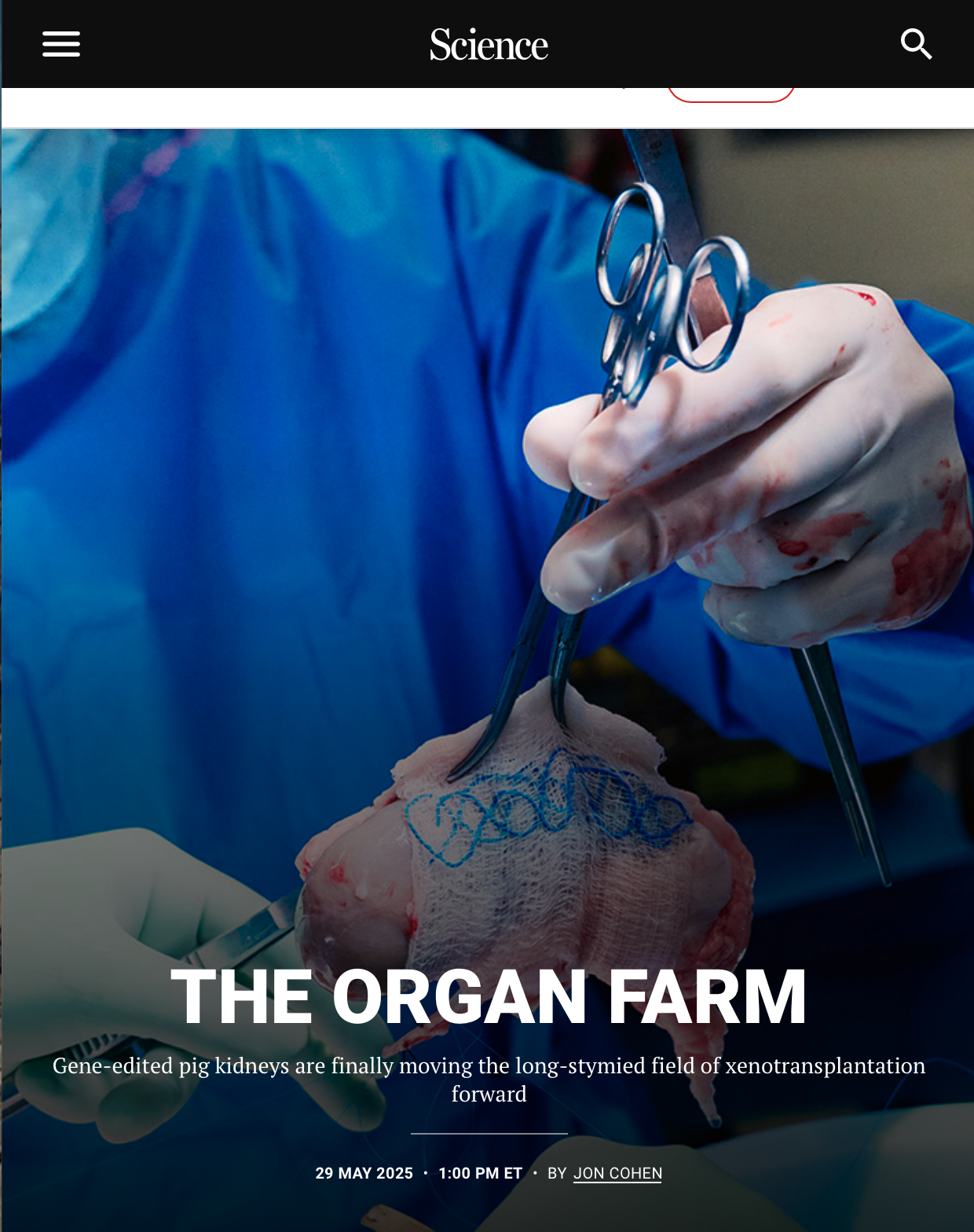
UAB awarded $19.5 million grant for new xenotransplantation program - UAB News - 2016
United Therapeutics Corporation - pipeline -> manufacturing organs for transplantation
Gene-Editing Success Brings Pig-to-Human Transplants Closer to Reality - CRISPR has enabled researchers to inactivate viruses in donor animals that may sicken humans - Scientific American - 2017
“The idea of solving the human organ shortage with pigs has tantalized surgeons for decades. More than 117,000 Americans are currently on a transplant wait-list in the U.S., according to federal figures, and 22 people die every day awaiting a match.
“Pig organs are similar in size and function to our own, and people are less squeamish about harvesting body parts from an animal raised for meat than they would be about a primate’s.Yet one major hurdle that has continued to vex any such cross-species transplants, or xenotransplants, has been the threat of transmitting viruses that can infect people and pigs alike: The latter’s genome includes 25 so-called retroviruses that apparently do nothing to porkers but might transmit diseases to people—especially immune-compromised transplant patients.
”That concern, particularly amid the HIV epidemic, has helped stall such research for the past couple decades (with the exception of pig heart valves that are used in humans—dead tissue that doesn’t pose the same transmission risks). Recent gene editing advances, however, are rejuvenating interest in pig-to-human transplants.”
Genome Editing with CRISPR-Cas9 - MIT video
What is CRISPR? - Bozeman Science video
Scientists grow bullish on pig-to-human transplants - Science AAAS - 2017
Porcine to Human Heart Transplantation - Is Clinical Application Now Appropriate? - C. McGregor , G. Byrne, UAB - review article - Journal of Immunology Research - 2017
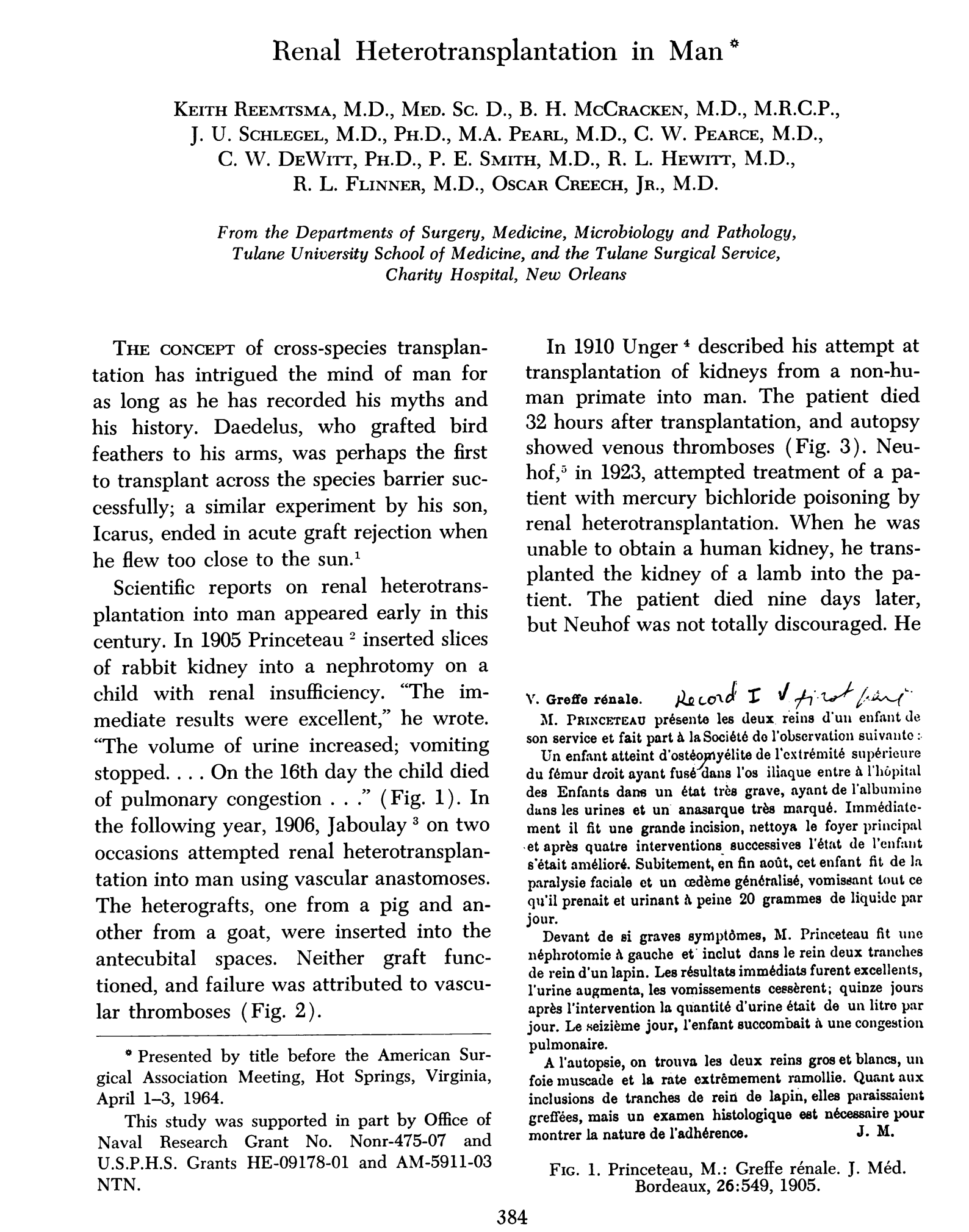
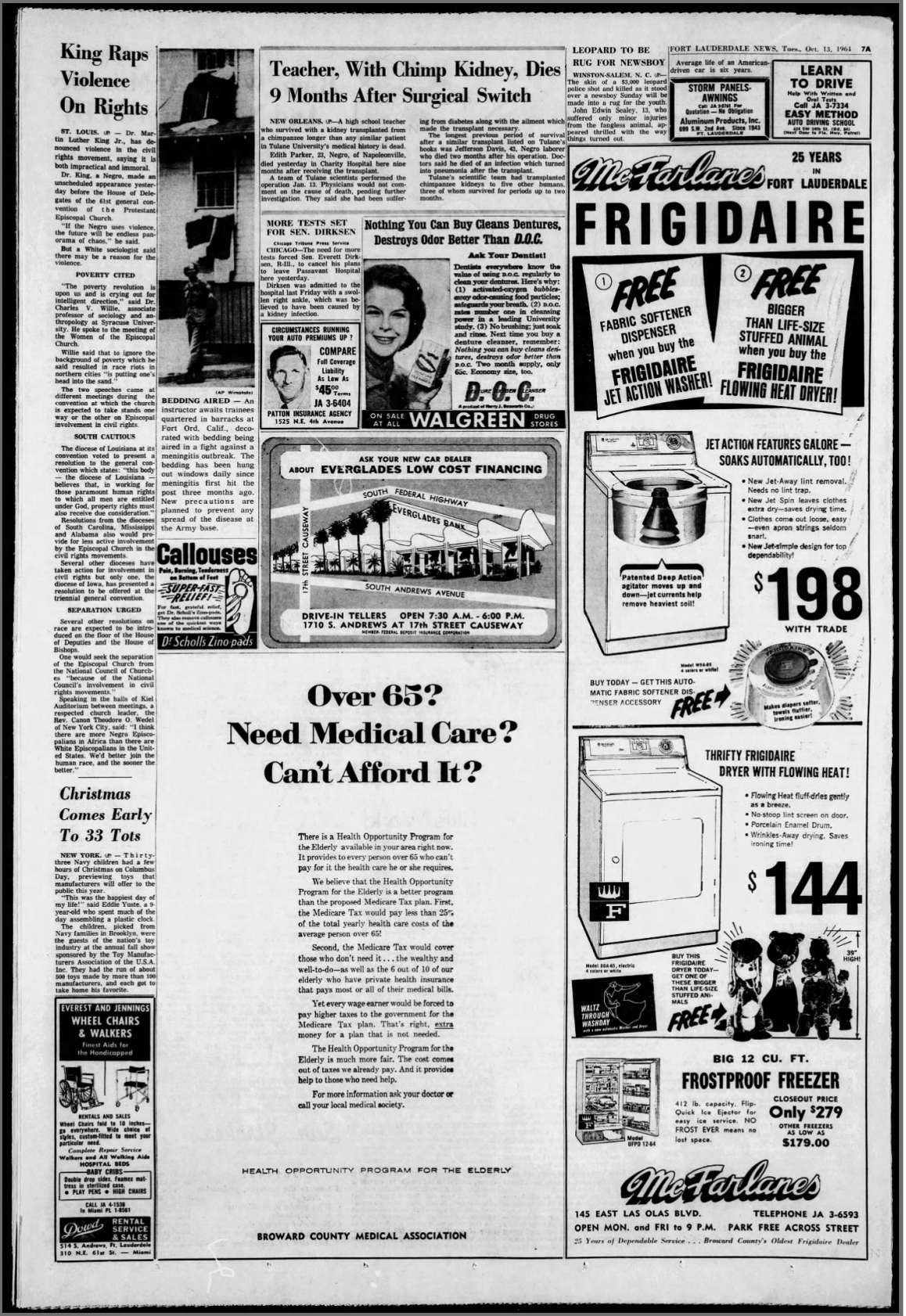
A brief history of cross-species organ transplantation - David Cooper - 2012
Neonatal pig hearts can heal from heart attack - Circulation 2018 - UAB News
Success for pig-to-baboon heart transplants - Nature - 12/5/18
This CEO is trying to genetically modify pig organs for human transplant - CNBC - 6/27/19
Google search: “UAB Xenotransplantation”
The Stanford Virtual Heart - cardiac VR imaging
Revolutionizing Heart Surgery with Virtual Reality - video
Heart: A History - Sandeep Jauhar - 2018
A History of the Heart, That Most Vital of Organs - NYT review of Jauhar’s book
“Be Careful, It’s My Heart” - video clip - Holiday Inn - 1942
Impella heart pump - temporary mechanical support for left ventricular cardiac output - info and video
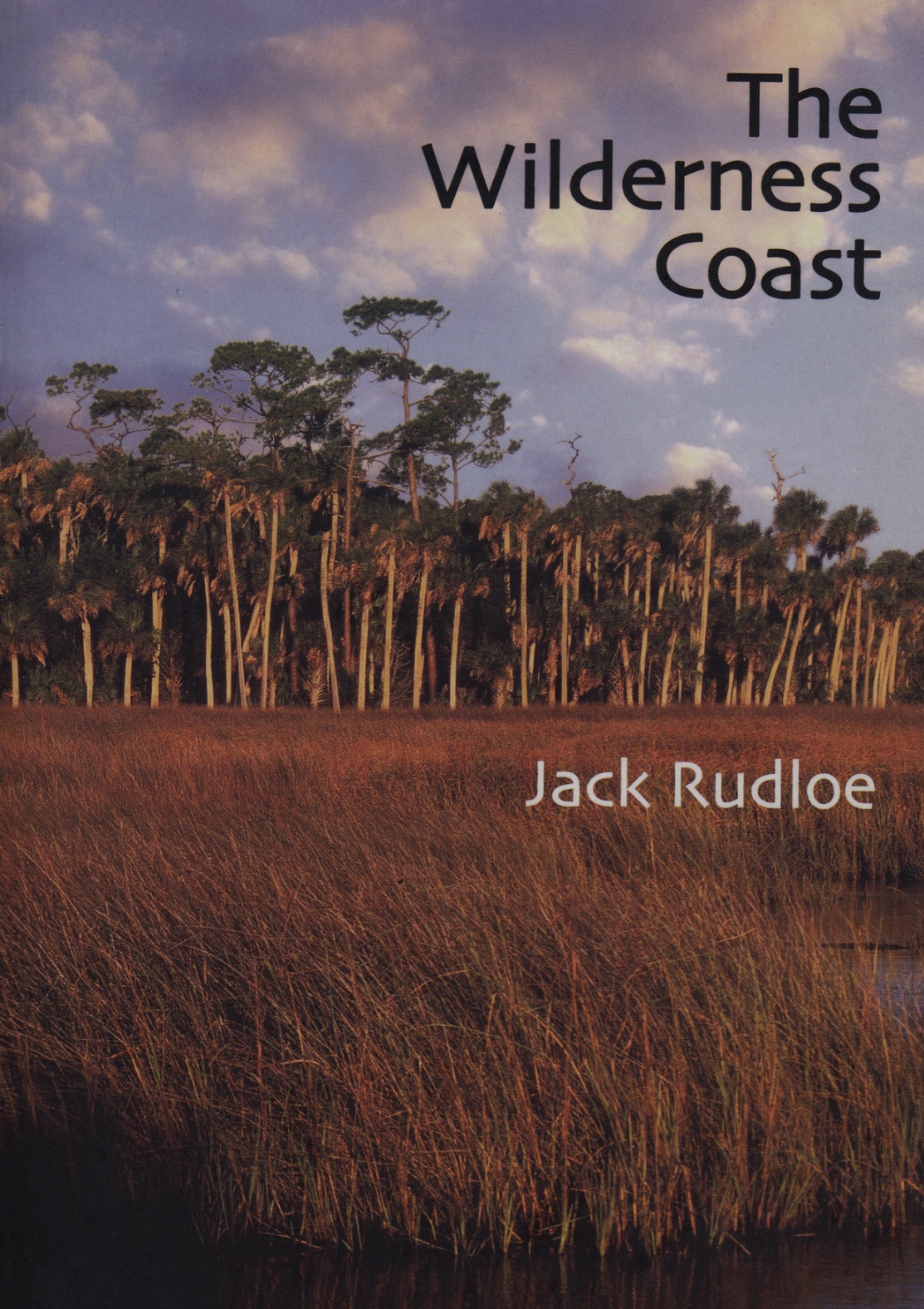
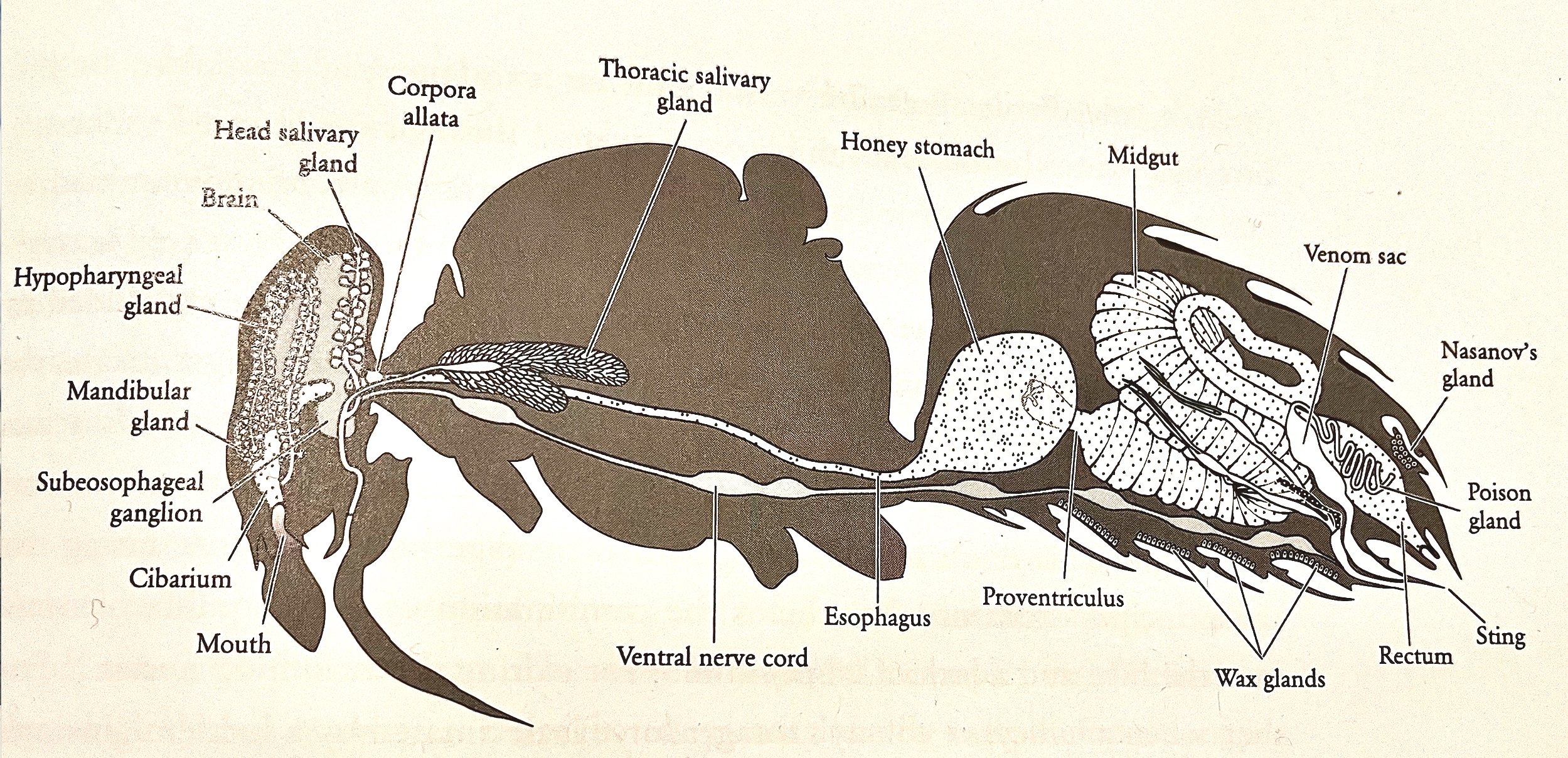
The Anatomy of the Honey Bee - 1910 - R. E. Snodgrass
Regulation of Heartbeat in the Honeybee - 1991 - Schwab et al.
Honeybee Heartbeat Modulation - 2011 - Papaefthimiou et al.


































































































































































![book info excerpts: He [Poggio Bracciolini] was a superbly well-trained scribe, with exceptionally fine handwriting, great powers of concentration, and a high degree of accuracy. It is difficult for us, at this distance, to take in](https://images.squarespace-cdn.com/content/v1/522b22f2e4b04879e6b51037/1611832427058-4P02RR9ZE3RDI40SYF1O/Screen+Shot+2021-01-28+at+4.55.03+AM.png)
































































































































































































![link to full text The Frank–Starling mechanism of the heart is due, in part, to modulation of myofilament Ca2+ sensitivity by sarcomere length (SL) [length-dependent activation (LDA)]. The molecular mechanism(s) that underlie LDA are unknown.](https://images.squarespace-cdn.com/content/v1/522b22f2e4b04879e6b51037/1735135358123-T6T1OTHHGDRL07BNM3FA/Screenshot+2024-12-25+at+8.02.18%E2%80%AFAM.png)


























































































































































































![PRIDE - 3.6.05, 0830h - Colorado R. - elev. 2400 ft. [1].jpg](https://images.squarespace-cdn.com/content/v1/522b22f2e4b04879e6b51037/1517996787739-IRVCCVHAXTQ161155JO0/PRIDE+-+3.6.05%2C+0830h+-+Colorado+R.+-+elev.+2400+ft.++%5B1%5D.jpg)
































![“ We performed the first coronary angioplasty [at UAB] in 1982, and the technology raced ahead in the years to follow. Particularly important was the development of the stent, a tiny spring ‘like that in your ball-point pen, only a bit larger,’ p](https://images.squarespace-cdn.com/content/v1/522b22f2e4b04879e6b51037/1596998467392-T37YI1NAKLYGVW2T44Z3/Screen+Shot+2020-08-09+at+1.39.09+PM.png)


























































![When Tinsley returned home to Birmingham for the Christmas holiday [1918], he had several long and serious conversations with his father. He was happy at Michigan; it was a good school. He was doing well, and it was certain that he would ob](https://images.squarespace-cdn.com/content/v1/522b22f2e4b04879e6b51037/1513633183575-Y7LE0P5CQTNGXXUCEYX5/Tinsley+Harrison+at+Vanderbilt.JPG)


























































![Dr. Eugene Braunwald is often called the father of modern cardiology. He calls that an exaggeration. [excerpt from 11/15/24 AHA News ] "Maybe I've been around longer, but there are a lot of people who have made major contributions to cardiology,"](https://images.squarespace-cdn.com/content/v1/522b22f2e4b04879e6b51037/1753740206960-EQJO36O2Q2O4L0C0PS9S/Screenshot+2025-07-28+at+4.57.32%E2%80%AFPM.png)






































































































































































































































































![Atrial repolarization wave (Ta wave) is usually not evident on the electrocardiogram (ECG) as it has a low amplitude of hundred to two hundred microvolts and is usually hidden in the QRS complex. [1] It can also extend into the ST segment caus](https://images.squarespace-cdn.com/content/v1/522b22f2e4b04879e6b51037/1650199590403-CJZ79M346S33E76PTQXK/Screen+Shot+2022-04-17+at+7.39.01+AM.png)






















































































































































































































































































![Claude Bernard 1813 - 1878 Milieu intérieur is the key process with which Bernard is associated. He wrote, "The stability of the internal environment [the milieu intérieur] is the condition for the free and independent life." This is the un](https://images.squarespace-cdn.com/content/v1/522b22f2e4b04879e6b51037/1576220108608-H880NXZ4F9MO4IUP0U6M/Screen+Shot+2019-12-13+at+12.54.44+AM.png)






























































































































































































































































































































































































































![full article excerpt: The biggest worry racing through the minds of ADL leaders [in 1960] was the reaction of the city's New Americans, as local Holocaust survivors were known. Members of the executive committee were all too familiar with](https://images.squarespace-cdn.com/content/v1/522b22f2e4b04879e6b51037/1682941623362-DNRAOROWDZY05WX42TJC/Screenshot+2023-05-01+at+6.45.02+AM.png)
























![[Dr. Ruth] Westheimer was born Karola Ruth Siegel to an Orthodox Jewish couple in the German town of Wiesenfeld. She was 10 years old when she was put on a train to Switzerland, part of the Kindertransport of Jewish children seeking](https://images.squarespace-cdn.com/content/v1/522b22f2e4b04879e6b51037/1699882886836-6JBSAJCCFE4X2MXUS8UC/rw.jpg)


























































































































































































































































































































































































































































































































































































































































































![“ We performed the first coronary angioplasty [ at UAB] in 1982, and the technology raced ahead in the years to follow. Particularly important was the development of the stent, a tiny spring ‘like that in your ball-point pen, only a bit large](https://images.squarespace-cdn.com/content/v1/522b22f2e4b04879e6b51037/1596755620909-1HRJBE6NLW8ZE6LCKP1P/IMG-7986.jpg)